Although it pains me to see how low the threshold is for defining “older women” in this research, I am glad to see that the findings of this longitudinal study confirm that the HPV vaccine is of little to no benefit to older women. The study was published in Journal of the National Cancer Institute last month.
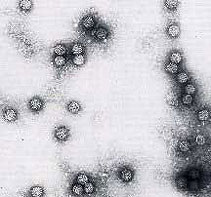
In a 7-year population-based cohort study in Costa Rica, the researchers looked at more than 9000 women in four age groups: ages 18–25, 26–33, 34–41, and ≥42 years to assess whether women’s age and the duration of carcinogenic HPV infections influenced subsequent persistence of infection and risk of cervical cancer. They found that regardless of the woman’s age, newly detected infections were associated with very low absolute risks of persistent infection or cancer.
Although cervical cancer is more common in older women, it usually develops many years – even decades – after exposure to a carcinogenic virus. The research team found that the rate of newly detected infections dropped with age — to 13.5 percent in women 42 and older, from 35 percent in women 18 to 25. In younger and older women alike, new infections generally cleared up without treatment.
The researchers concluded that the potential benefitof prophylactic vaccination or frequent HPV screening to prevent or detect new carcinogenic HPV infections is low in women aged 34 years and older.


Great. Just as the vaccine has been approved for older women, the proof comes that it is a waste of money. May the “push to precribe” be dealt a big push back.
The point is that the Merck funded the studies stating that HPV works for older
women. The Costa Rica study is an independent study – and that is why it is
valuable. Also interesting to note that another Merck funded study supports
vaccine use for men with HIV/AIDS. Yet in the PPI – women with HIV/AIDS are told to
report this condition to their doctor prior to vaccination.