by Heather Dillaway | Aug 22, 2014 | Hormones, magazines, Media, Men, Pharmaceutical
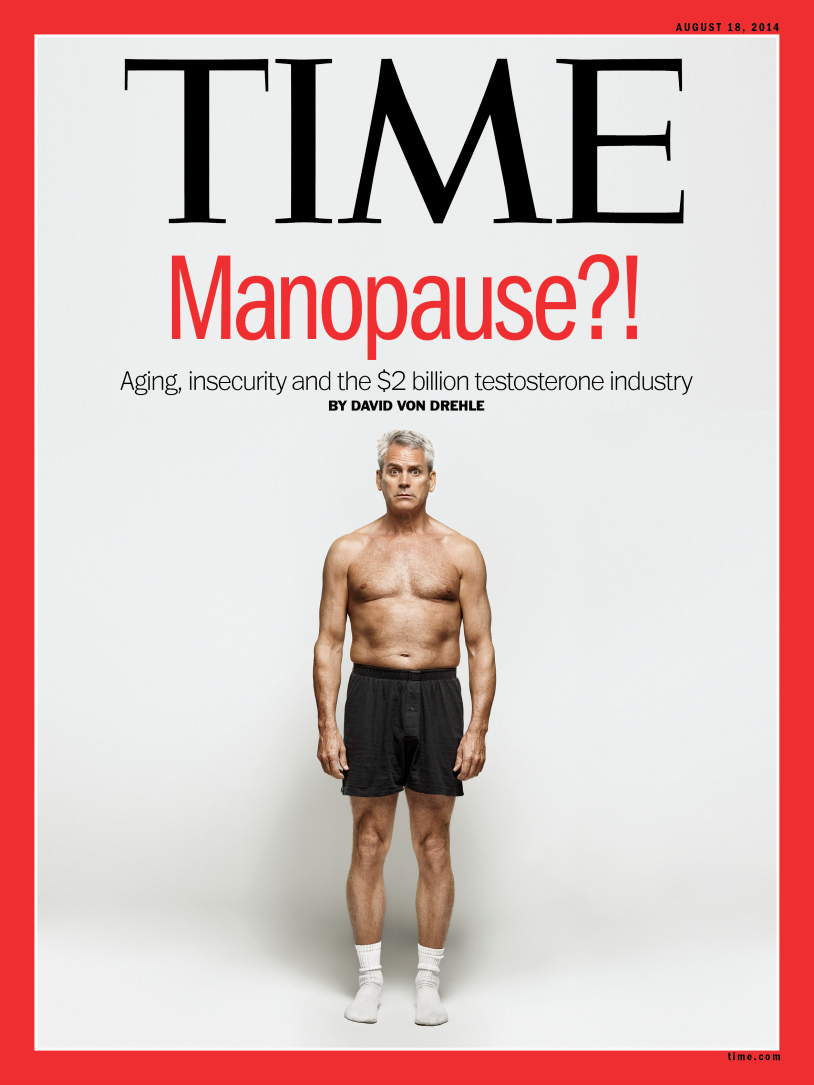
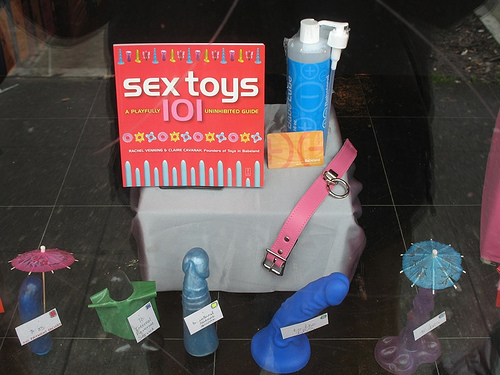
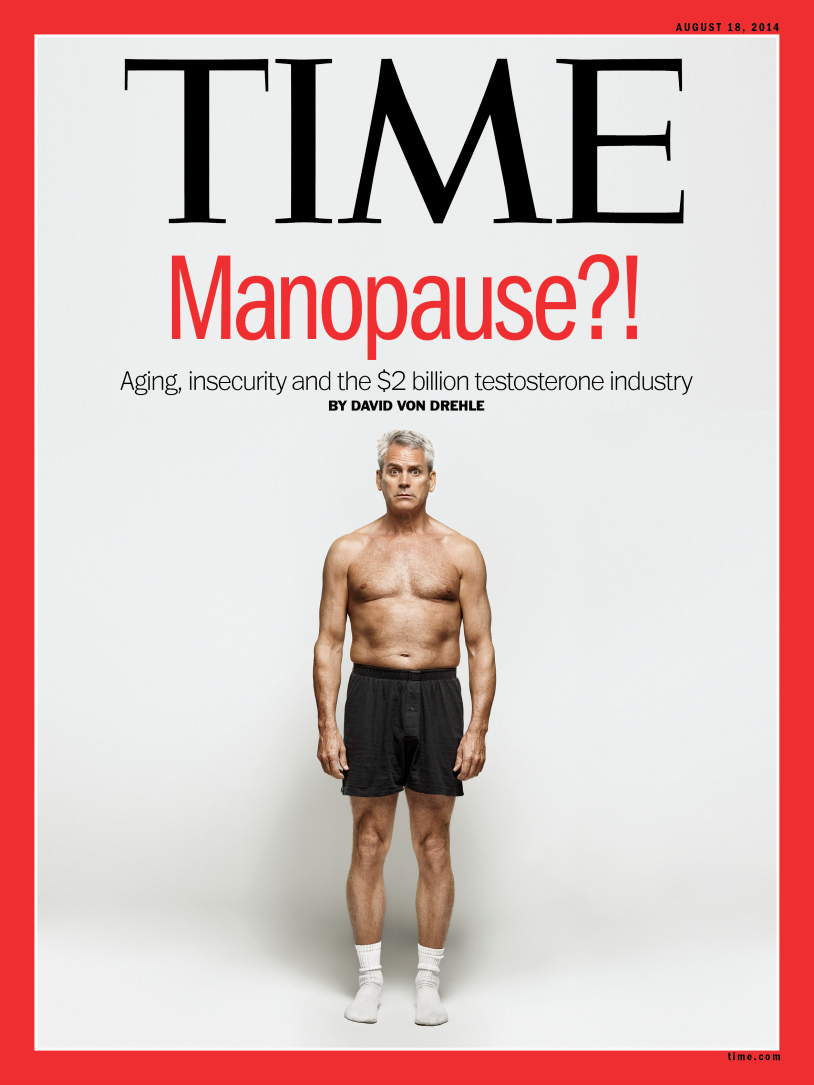
By now, everyone has probably seen this week’s TIME cover story. The magazine’s August 18th cover photo showed a topless, seemingly frumpy, middle-aged man worried about his loss of testosterone and (therefore) manhood under the title, “Manopause?! Aging, Insecurity...
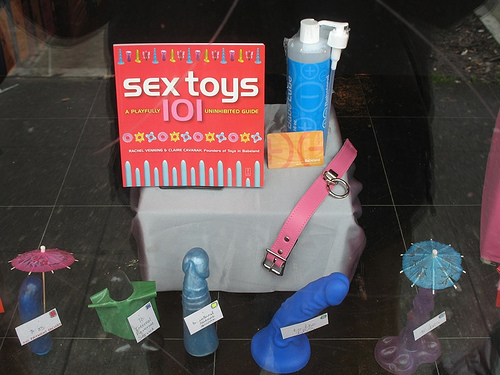
by Elizabeth Kissling | Oct 26, 2012 | Birth Control, DIY, Sex
Guest Post by Holly Grigg-Spall, Sweetening the Pill At the West Coast Catalyst Convention for sex-positive sex-educators I was listening to a talk on definitions of sexual health when the birth control pill was brought up. I’d spent much of the event feeling...

by Laura Wershler | May 17, 2010 | Birth Control, Men, New Research, Pharmaceutical, Reproduction
You know how most superheros become superheros because of exposure to some weird, intensified chemical or element? Take Peter Parker’s spider bite for example. According to a story reported in various media, including International Planned Parenthood...