by Laura Wershler | Jul 23, 2015 | Ovulation
Everybody seems to be talking about ovulation these days in one context or another. ScienceDaily reported that women’s faces get redder when they ovulate, but it is imperceptible to the human eye. The Pharmaceutical Journal reported on a small study that showed...
by Editor | Jul 11, 2015 | FemCare, Ovulation, Reusable menstrual products
1. Naturopathic Doctor Lara Briden explains 4 Causes of Androgen Excess in Women on her Healthy Hormone Blog this week. If you are experiencing hair loss, facial hair (hirsutism) or acne, or have been diagnosed with PCOS, you’ll want to check this out for a...
by Saniya Lee Ghanoui | Feb 2, 2015 | Art, Menstruation, Ovulation, Sports
Guest Post by Dana Michelle Gillespie Editor’s Note: This blog cross-posted from Pole World News. Pole dancing has quickly become one of the most internationally sought after fitness, sports, and art forms in the world. The pole movement craze is a rapidly...
by Kati Bicknell | Nov 20, 2012 | Fertility, Menstruation, Ovulation
Have you ever been concerned because your period was late? I know I have. But I’m not anymore! And you don’t have to be either! And since I’m sure you’d rather not spend several days every month nervously pacing and counting dates backwards on your hands while glaring...

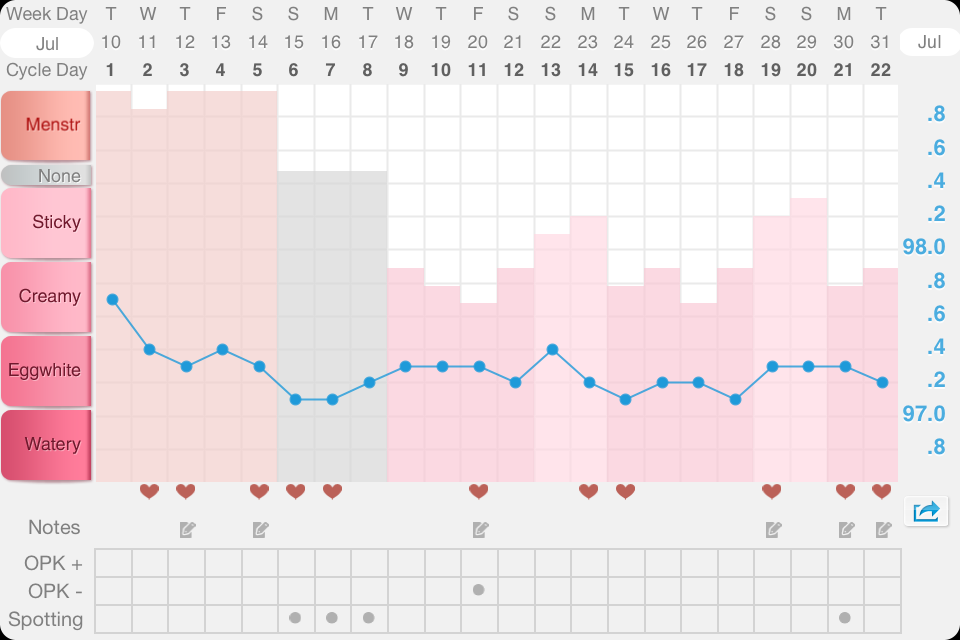
by Kati Bicknell | Jul 31, 2012 | Fertility, Ovulation
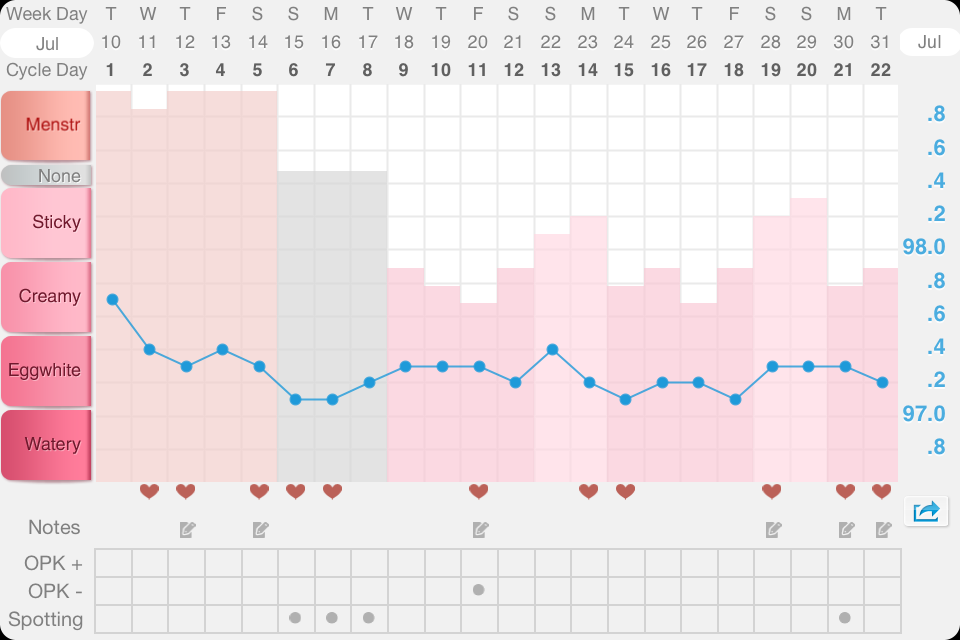
I’ve been doing research on my own menstrual cycle for almost four years, charting my cycle using the Fertility Awareness Method. My cycles have always been wacky. I got my period when I was 11 but bled only a couple times a year, until, at my doctor’s...