by Holly Grigg-Spall | Jun 4, 2013 | Activism, Birth Control, Girls, Health Care, Hormones, Menstruation
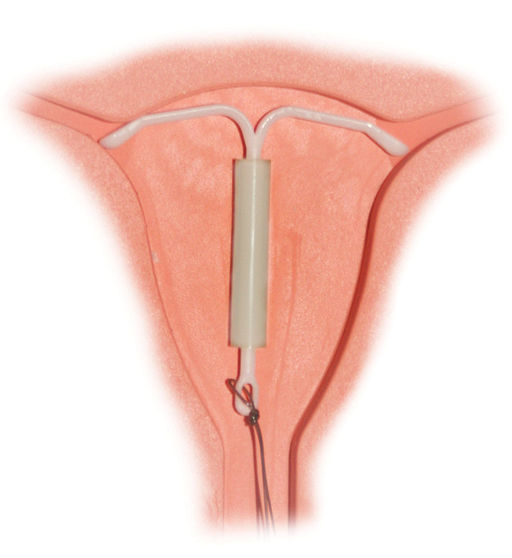
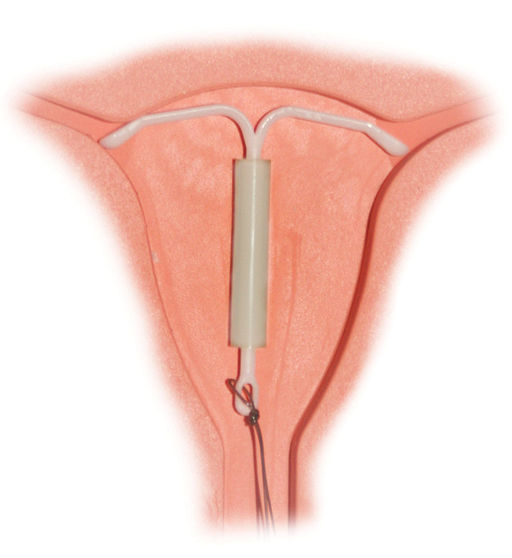
Do women using the Mirena hormonal IUD have their period? Does it suppress the hormone cycle for all women or just some? How does it work to prevent pregnancy exactly? It seems these questions can’t be answered even by the assumed experts. We are told the Mirena...
by Laura Wershler | Dec 12, 2012 | Activism, Birth Control, Coming off the pill, Girls, Health Care, Hormones, Politics
Throughout the contraceptive realm, LARCs are being heralded as the best thing since Cinderella’s glass slipper with little acknowledgement that for many women LARCs are more like Snow White’s poisoned apple. Nov. 25 to Dec. 1, 2012, was LARC Awareness...
by Elizabeth Kissling | Jul 8, 2010 | Birth Control, Dysmenorrhea, Girls, Health Care, Menorrhagia, New Research, Pharmaceutical
A new study published in the Journal of Obstetrics and Gynecology has found that adolescents are usually able to tolerate the Mirena® IUD rather well. The mean age of girls in this British study was 15.3 years, and they were prescribed the Mirena® for painful and/or...
by Chris Hitchcock | Apr 20, 2010 | Birth Control, Health Care, Menstruation, Ovulation, Pharmaceutical, Reproduction, Sex
It’s starting. With the approaching 50th anniversary of the birth control pill, there will be a flood of anniversary celebrations and reviews of birth control methods. Which is good. We should have those discussions more often. Just say “no” (on the...