by Laura Wershler | Dec 12, 2012 | Activism, Birth Control, Coming off the pill, Girls, Health Care, Hormones, Politics
Throughout the contraceptive realm, LARCs are being heralded as the best thing since Cinderella’s glass slipper with little acknowledgement that for many women LARCs are more like Snow White’s poisoned apple. Nov. 25 to Dec. 1, 2012, was LARC Awareness...
by Elizabeth Kissling | Oct 26, 2012 | Birth Control, DIY, Sex
Guest Post by Holly Grigg-Spall, Sweetening the Pill At the West Coast Catalyst Convention for sex-positive sex-educators I was listening to a talk on definitions of sexual health when the birth control pill was brought up. I’d spent much of the event feeling...
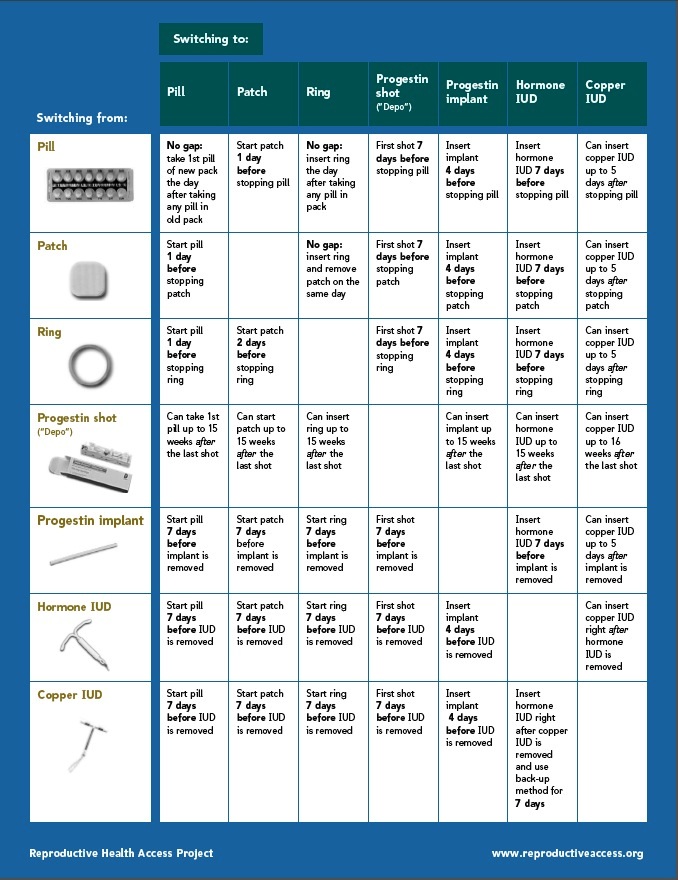
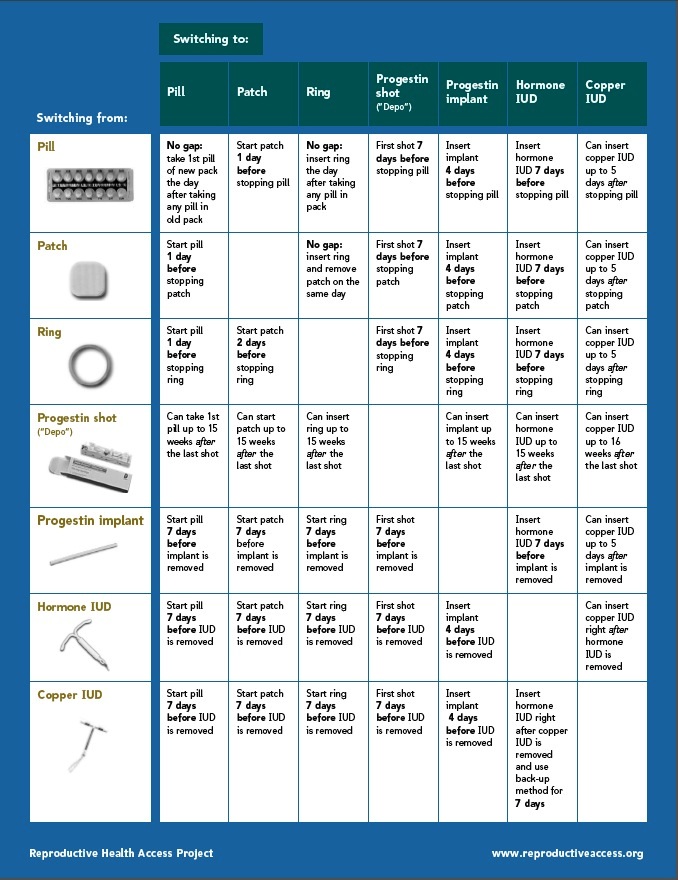
by Laura Wershler | Oct 17, 2012 | Activism, Birth Control, Coming off the pill, Health Care, Menstruation, Pharmaceutical
Birth control in the U.S. has become synonymous with drugs and devices. The pill, patch, or ring; Depo-Provera or hormonal implant; copper IUD or Mirena IUD; traditional hormonal birth control or long-acting reversible contraceptives. All impact the function of the...