by Laura Wershler | Feb 5, 2014 | Birth Control, Books, Celebrities, Health Care, Hormones, Menstruation, Ovulation
I was curious. If Cameron Diaz’s purpose in writing The Body Book: The Law of Hunger, the Science of Strength, and Other Ways to Love Your Amazing Body was empowerment, helping women to understand how their bodies work, would she include information about the...

by Laura Wershler | Jan 10, 2014 | Birth Control, Coming off the pill, Fertility, Menstruation, Ovulation
A month ago I was musing about what it might be like to blog about fun stuff like food, fashion or travel – you know, topics not quite so “fraught” as the menstrual cycle. Sometimes it feels like just so much work sharing facts and opinions about why body...
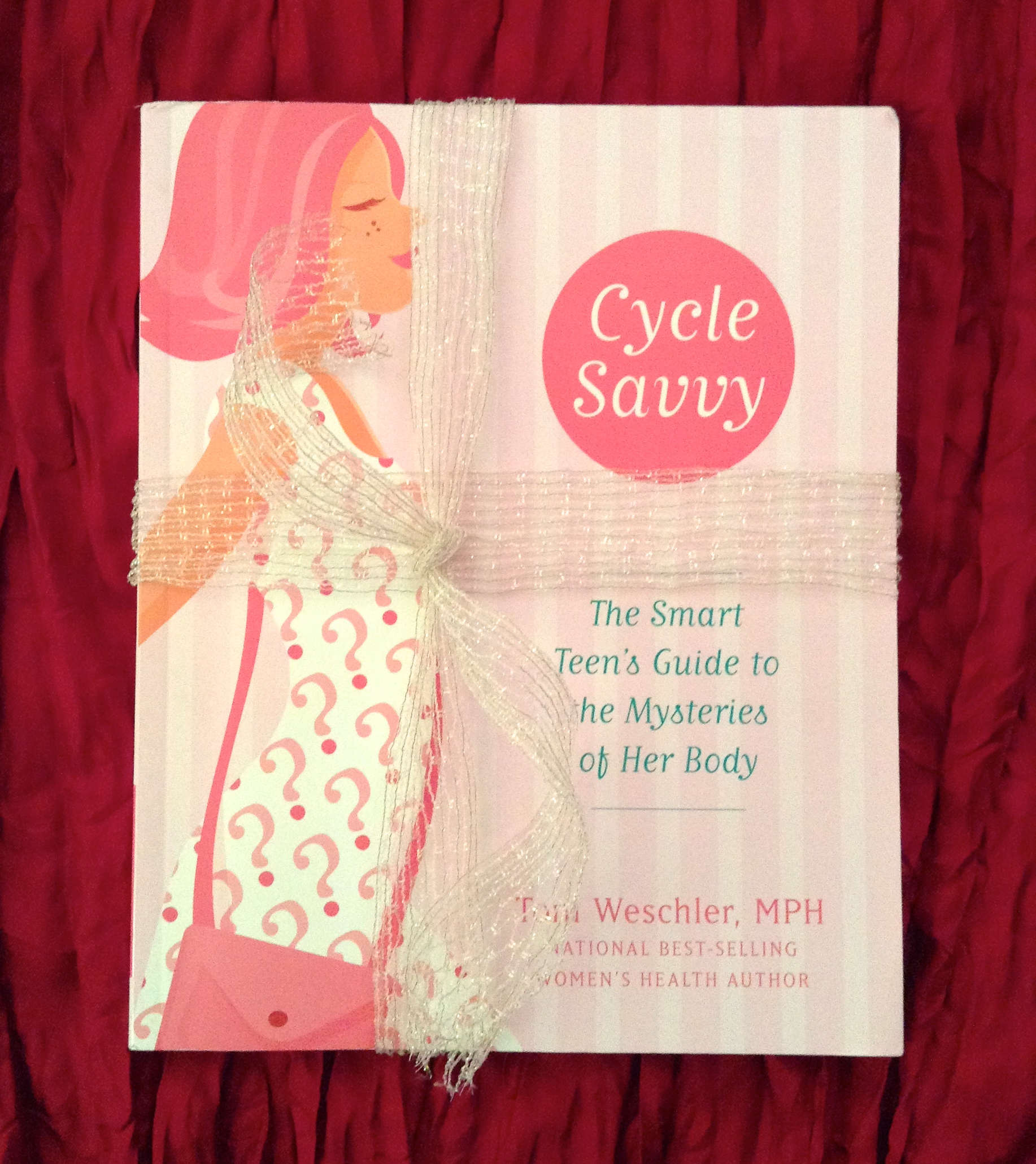
by Laura Wershler | Dec 16, 2013 | Birth Control, Books, Fertility, Girls, Menarche, Menopause, Menstruation, Perimenopause
This holiday season consider giving the women in your life the gift of body literacy. The books, resources and services compiled below support understanding and appreciation of our bodies. Gifts for teenagers: * To hold a Wondrous Vulva Puppet is to experience a...
by Laura Wershler | Nov 13, 2013 | Activism, Birth Control, Coming off the pill, Hormones, Menstruation, Radio
Questioning and quitting the pill are current hot topics, fueled in no small part by Holly Grigg-Spall’s recently released Sweetening the Pill Or How We Got Hooked on Hormonal Birth Control. Her book has drawn ample backlash, brilliantly addressed by re:Cycling...
by Laura Wershler | Oct 16, 2013 | Activism, Birth Control, Books, Coming off the pill, Health Care, Hormones, Menstruation, Ovulation, Pharmaceutical
I had the privilege of writing the foreword for Holly Grigg-Spall’s recently published book Sweetening the Pill: Or How We Got Hooked on Hormonal Birth Control. It’s astounding to me that more than 30 years ago, before Holly was born, I was asking some of...