by Paula Derry | Nov 11, 2013 | Health Care, Menopause
Does menopause cause an increase in health problems ranging from heart disease to bone disease to psychological depression? One issue is that many of these claims have been criticized as being overblown both by professionals within the medical community and by critics...
by Paula Derry | Oct 15, 2012 | Menopause, New Research
Many of us do our own health research, either because we have a specific question or simply to keep up with the news. If we don’t read the original scientific articles, we rely on experts to provide summaries in newspapers, magazines, or on a variety of websites. It...
by Paula Derry | Aug 27, 2012 | Menopause, New Research
A recent article by Swift et al. looked at the effects of aerobic exercise on heart health. Midlife women with high blood pressure were assigned to one of three exercise groups—a program of exercise that met National Institutes of Health (NIH) guidelines, one that was...
by Laura Wershler | Feb 8, 2012 | Advertising, Communication, Health Care, magazines, Menopause, Television
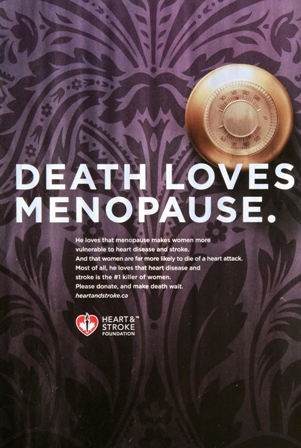
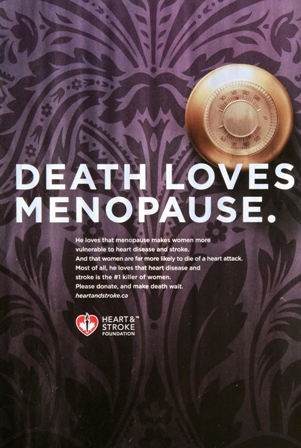
The Heart and Stroke Foundation of Canada has inaccurately branded menopause as a killer of women. I will not be sending them a donation. Last October, the foundation launched a fundraising campaign called Make Death Wait. Magazine and TV ads personify death as a man...
by Chris Hitchcock | Sep 27, 2011 | Menopause, New Research
Earlier this month, researchers published a statistical analysis of mortality data in England, Wales and the United States, disproving the common statement that, after menopause, women face increased rates of mortality from heart disease. There are other studies that...