by Holly Grigg-Spall | Apr 8, 2014 | Amenorrhea, Birth Control, Celebrities, Coming off the pill, Communication, Disposable menstrual products, FemCare, Health Care, Menarche, Menstruation, Pharmaceutical, Politics, Reusable menstrual products
A few weeks back I did an interview with Leslie Botha regarding the distribution of Depo Provera to women in developing countries. Recently Leslie shared with me an email she received from someone working in a family planning clinic in Karnataka, India. He described...
by Laura Wershler | Feb 6, 2013 | Activism, Amenorrhea, Birth Control, Coming off the pill, Health Care, Hormones, Menstruation, Pharmaceutical
Author’s Update, February 14, 2013: As clarified by Bedsider.org in the comments section below, the Works Like A Charm Contest mentioned in this post is not current but ended in 2011. The contest website pages are now inactive. If Bedsider.org sponsored a...

by Laura Wershler | Jan 9, 2013 | Activism, Amenorrhea, Birth Control, Communication, Health Care, Menstruation, Ovulation
As 2013 begins, I give thanks to each and every one of my colleagues at the Society for Menstrual Cycle Research and all my blogging buddies at re:Cycling. Without them I’d feel left out in the cold. I’ve been a menstrual cycle advocate since 1979 when,...
by Laura Wershler | Mar 7, 2012 | Activism, Amenorrhea, Birth Control, Coming off the pill, Communication, Dysmenorrhea, Health Care, Hormones, Menorrhagia, Menstruation, Ovulation, Pharmaceutical, PMS, Reproduction
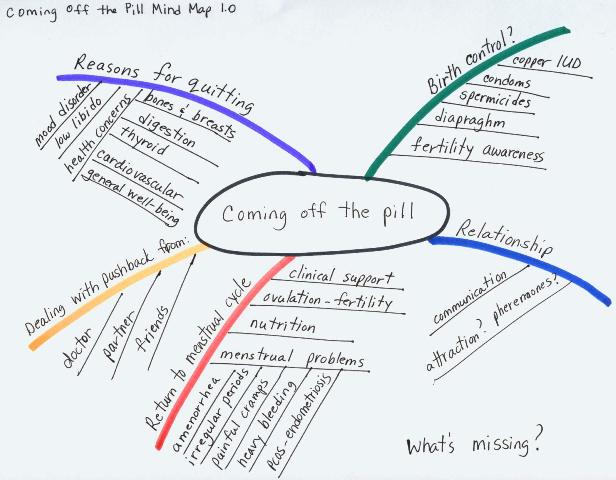
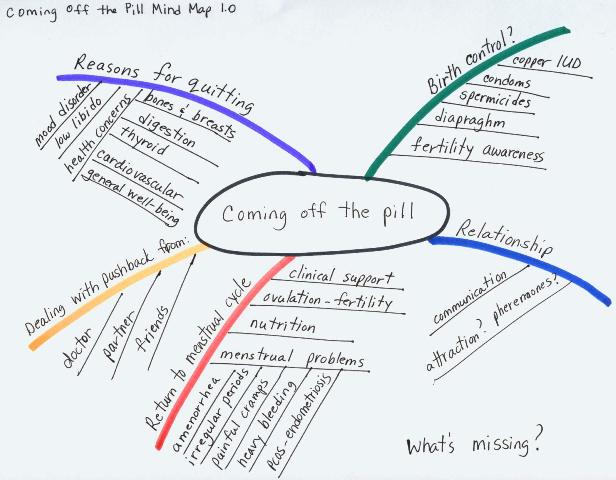
Everybody can use a good map to help them get to where they’re going. Why not women heading to the land of non-hormonal contraception? In my post on January 11, 2012 I asked if coming off the pill was a growing trend. I proposed to write a series of posts about...

by David Linton | Jan 18, 2012 | Amenorrhea, Menstruation, Sports
Guest Post by Lianne McTavish — University of Alberta (aka Feminist Figure Girl) While working out at the gym yesterday—something I do on a daily basis—I felt a strangely familiar pressure in my lower abdomen and noticed that it was protruding, despite the...
by Elizabeth Kissling | Sep 2, 2010 | Amenorrhea, Health Care, Media, Menstruation
The headline of a story at ABC news about infertility among female athletes is “Female Athletes Are Too Fit To Get Pregnant“. Many women athletes in their 20s, at peak performance levels and peak physical fitness by most measures, may find themselves...