by Editor | Sep 12, 2016 | Menopause, Perimenopause, Sociology
Heather Dillaway, PhD, Professor of Sociology and Associate Dean, College of Liberal Arts & Sciences, Wayne State University When and why did you join the Society for Menstrual Cycle Research? I joined in spring 2004 and attended my first SMCR conference in 2005...

by Editor | Jun 23, 2016 | Ovulation, Perimenopause, Research
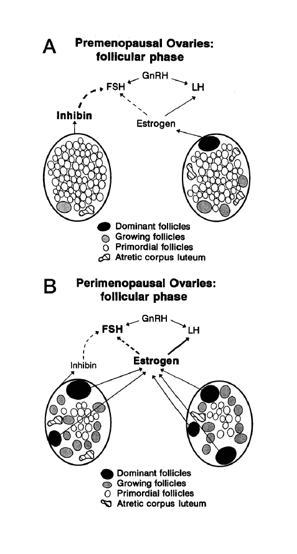
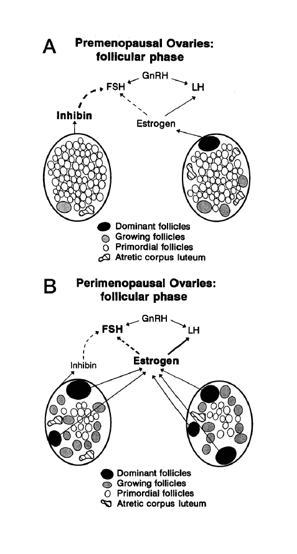
Jerilynn C. Prior BA, MD; Professor of Medicine/Endocrinology at the University of British Columbia; Scientific Director of the Centre for Menstrual Cycle and Ovulation Research When and why did you join the Society for Menstrual Cycle Research? I joined SMCR at the...
by Editor | Apr 28, 2016 | Menopause, Perimenopause
Writing Menopause, a diverse literary collection about menopause to be published in the spring of 2017 by Inanna Publications, was first introduced to the Society for Menstrual Cycle Research in a session presented at our June 2015 biennial conference in Boston. The...
by Editor | Apr 26, 2016 | Books, Literature, Menopause, Perimenopause
Writing Menopause, a diverse literary collection about menopause to be published in the spring of 2017 by Inanna Publications, was first introduced to the Society for Menstrual Cycle Research in a session presented at our June 2015 biennial conference in Boston. The...
by Editor | Apr 5, 2016 | Health Care, Menopause, Perimenopause
Making sense of the many names for women’s reproductive aging by Dr. Jerilynn C. Prior Jerilynn C. Prior BA, MD, FRCPC, ABIM, ABEM is a Professor of Endocrinology and Metabolism at the University of British Columbia in Vancouver, B.C. She is the founder (2002) and...
by Editor | Apr 27, 2015 | Literature, Menopause, Perimenopause, Sex
Three paper presentations on Menopause at the 21st Biennial Conference of the Society for Menstrual Cycle Research at The Center for Women’s Health and Human Rights, June 4-6, 2015, Suffolk University, Boston will explore sexuality and the menopausal woman, as well as...