Plastic Bodies: Women as malleable objects
SMCR member Emilia Sanabria digs deep into Brazilian attitudes and cultural approaches to women's bodies in her book Plastic Bodies: Sex Hormones and Menstrual Suppression in Brazil. Published by Duke University Press (2016), the book is described as follows:...

Battle Over Free Sanitary Pads Lands Ugandan Activist In Jail
A good deal of media exposure has been given to efforts in Canada, the United States, Australia, and Britain to eliminate menstrual product sales taxes and to provide pads and tampons in schools, prisons, and homeless shelters. However, there has been less attention...

Sustainable Cycles Rides Again: #SMCR2017
Guest Post by Rachel Saudek Starting April 1, 2017, a posse of spokes-women will begin the journey to the #SMCR2017 Conference happening June 22-24 in Atlanta, Georgia. Yes, we're a few months early, but that's because we are travelling by bicycle. We at Sustainable...
Endometriosis research and technology update
Today, one in ten women are living with endometriosis. You don't need to look far to find a Tweet, Facebook post or blog entry by someone you know living with the disease. So far in 2017, when it comes to endometriosis, patient advocacy, storytelling and education is...

Endometriosis, painful sex, and physical therapy
Guest Post by Dr. Sallie Sarrel, PT, ATC, DPT NOTE: This post was originally published on this blog on March 17, 2016. "We have emerged from the days of Freud and finger pointing that sexual pain is only psychological. Especially in the case of women with...
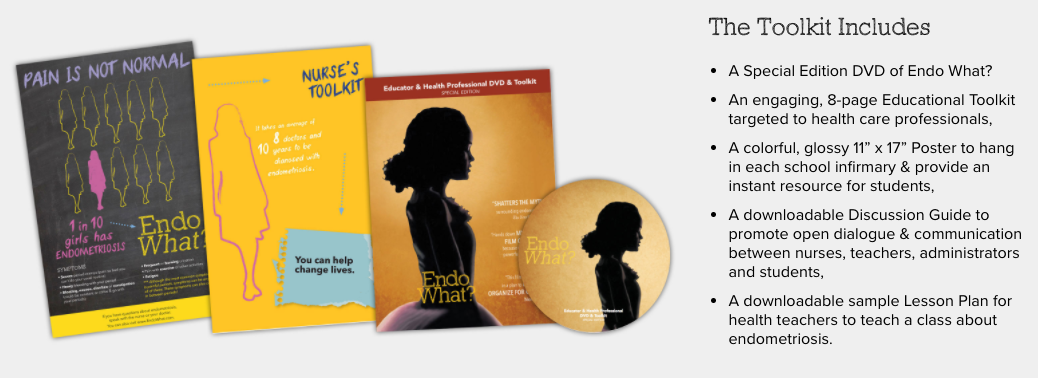
School nurse initiative launches with Endometriosis Awareness Month
Endo What?, the groundbreaking documentary about endometriosis, premiered in March 2016 to mark Endometriosis Awareness Month. Menstruation Matters reviewed the film on March 31, 2016, under the headline "Endo What? documentary sets the record straight about...

