by Laura Wershler | Mar 1, 2017 | Endometriosis, Independent Film, Menstrual education
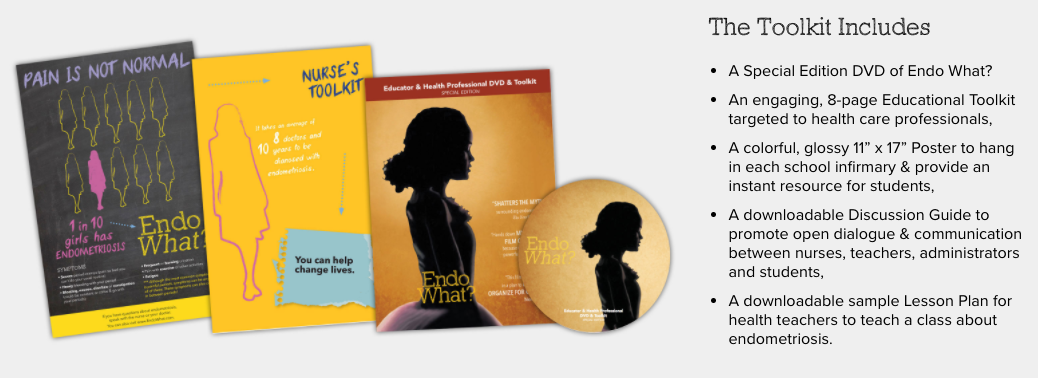
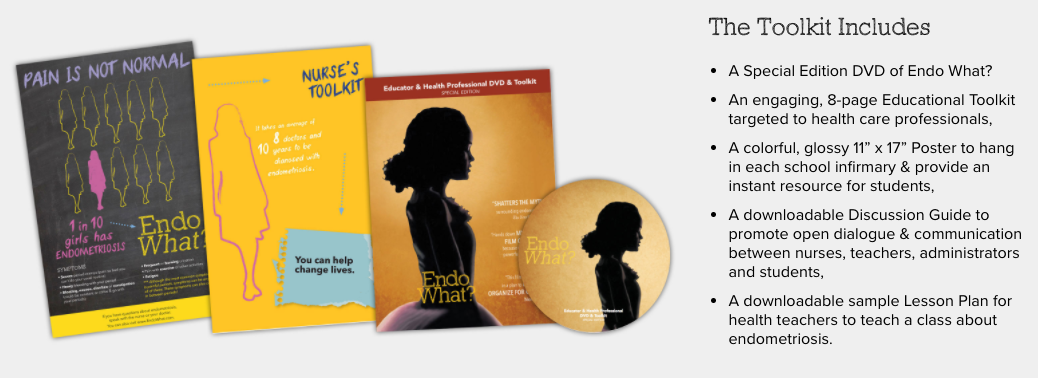
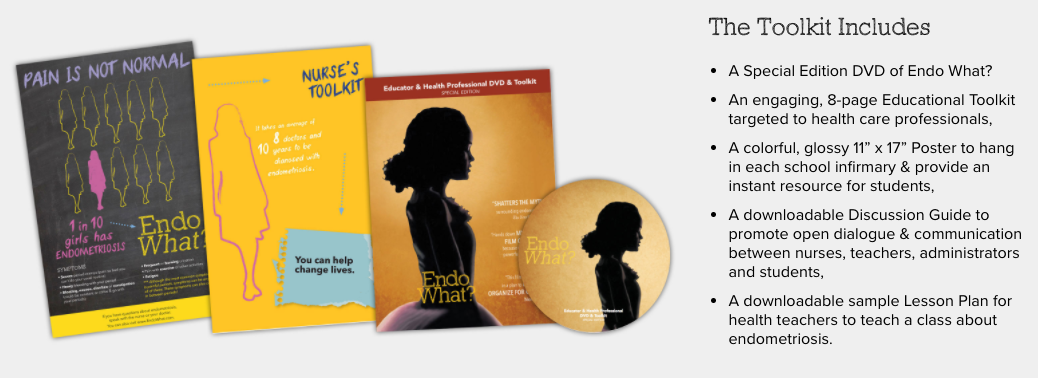
Endo What?, the groundbreaking documentary about endometriosis, premiered in March 2016 to mark Endometriosis Awareness Month. Menstruation Matters reviewed the film on March 31, 2016, under the headline “Endo What? documentary sets the record straight about...

by Laura Wershler | Feb 23, 2017 | Menstrual education
Fertility awareness educators and menstrual cycle healthcare providers are invited to share their expertise, experiences, and best practices at the Justisse Fertility Awareness Educators Conference in Nanaimo, British Columbia, August 23 to 27, 2017. With the rising...

by Laura Wershler | Jul 6, 2016 | Psychology, Research
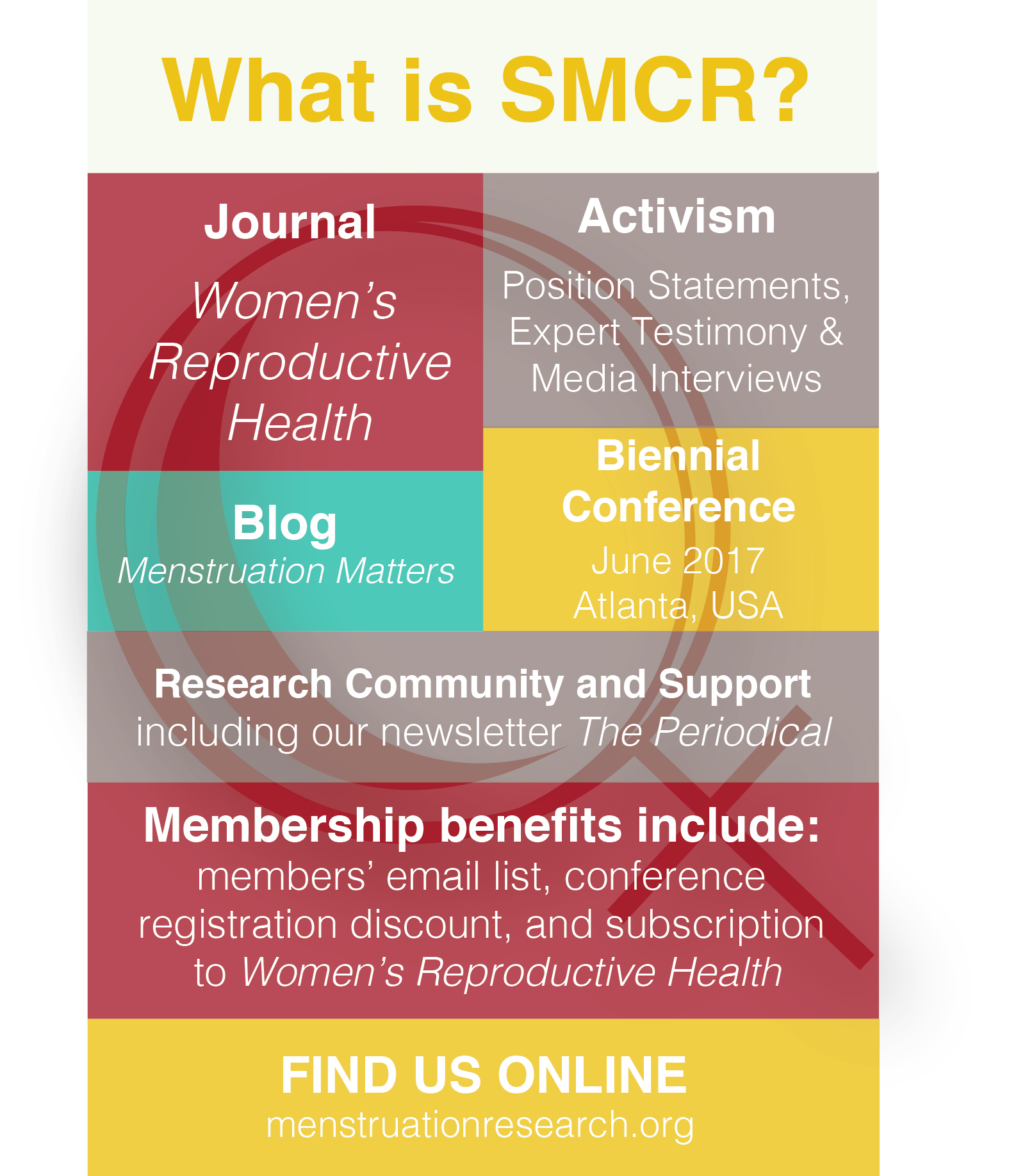
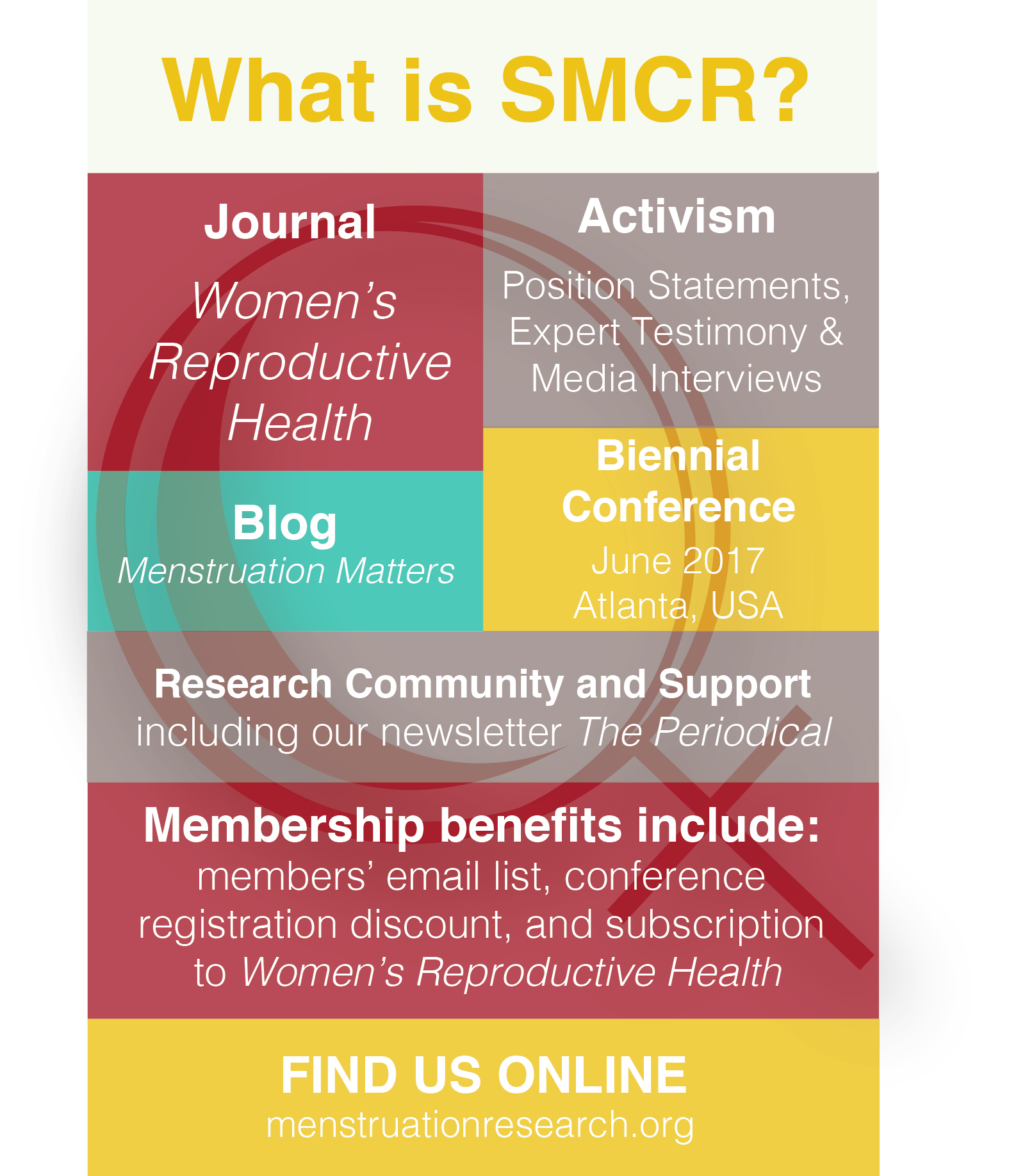
Jessica Barnack-Tavlaris, PhD, Assistant Professor, Department of Psychology, The College of New Jersey My PhD is in Experimental Health/Social Psychology, and I have a Master’s Degree in Public Health Specializing in Epidemiology When did you join the Society...
by Laura Wershler | May 28, 2016 | Menstruation
May 28 is Menstrual Hygiene Day. All over the world events are planned in honor of this year’s theme: Menstruation matters to everyone, everywhere. May 28, 2016, also marks the date that re: Cycling, the blog of the Society for Menstrual Cycle Research, gets...
by Laura Wershler | Apr 21, 2016 | Activism, magazines, Media
The menstrual advocacy movement splashes red all over the cover of Newsweek’s upcoming April 29, 2016 edition. The story by Abigail Jones–The Fight to End Period Shaming is Going Mainstream–published online April 20, 2016, continues the mad rush of...