April 14, 2015
We wish to thank all the women who’ve shared their experiences with Depo-Provera in the two years since this blog post was published. Comments are now closed.
Those concerned about Depo-Provera and bone density may want to read Dr. Prior’s article on Depo-Provera Use and Bone Health recently posted on the website of the Centre for Menstrual Cycle and Ovulation Research.
Laura Wershler and Dr. Jerilynn C. Prior
Laura Wershler interviews Ask Jerilynn, clinician-scientist and endocrinologist
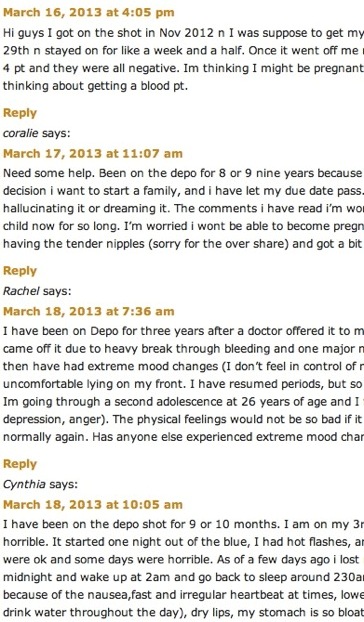
A screen shot of comments to Laura Wershler’s blog post of April 4, 2012: “Coming off Depo-Provera can be a woman’s worst nightmare.”
With 250 comments – and counting – to my year-old post Coming off Depo-Provera is a women’s worst nightmare (April 4, 2012) I thought it was time to revisit this topic.
That blog post has become a forum for women to share their negative experiences with stopping Depo-Provera (also called “the shot,” or Depo), the four-times-a-year contraceptive injection. (Commenters reporting positive experiences have been extremely rare.) Many women have experienced distressing effects either while taking Depo and/or after stopping it. They report that health-care professionals seem unable to explain their problems or to offer effective solutions. What is puzzling for many is why they are experiencing symptoms like sore breasts, heavy and ongoing bleeding (or not getting flow back at all), digestive problems, weight gain and mood issues when they stop Depo.
This post aims to briefly explain how Depo works to prevent pregnancy, its common side effects and, most importantly, why and what to do about adverse experiences when stopping it.
What follows is my interview with Dr. Jerilynn C. Prior, Society for Menstrual Cycle Research board member, professor of endocrinology at the University of British Columbia, and scientific director of the Centre for Menstrual Cycle and Ovulation Research (CeMCOR) Section 1 explains how Depo-Provera works and what causes its side effects. Section 2 explains the symptoms women are experiencing after stopping the drug.
1) Taking Depo-Provera: How it works and established side effects
Laura Wershler (LW): Dr. Prior, what is Depo-Provera® and how does it prevent pregnancy?
Ask Jerilynn: The term, “depo” means a deposit or injection and Provera is a common brand name of the most frequently used synthetic progestin in North America, medroxyprogesterone acetate (MPA). Depo is a shot of MPA given every three months in the large dose of 150 mg. Depo prevents pregnancy by “drying up” the cervical mucus so sperm have trouble swimming, by thinning the endometrium (uterine lining) so a fertilized egg can’t implant and primarily by suppressing the hypothalamic and pituitary signals that coordinate the menstrual cycle. That means a woman’s own hormone levels become almost as low as in menopause, with very low progesterone and lowered estrogen levels.
LW: Could you explain the hormonal changes behind the several established side effects of Depo? Let’s start with bleeding issues including spotting, unpredictable or non-stop bleeding that can last for several months before, in most women, leading to amenorrhea (no menstrual period).
Ask Jerilynn: It is not entirely clear, but probably the initial unpredictable bleeding relates to how long it takes for this big hormone injection to suppress women’s own estrogen levels. The other reason is that where the endometrium has gotten thin it is more likely to break down and bleed. These unpredictable flow side-effects of Depo are something that women should expect and plan for since they occur in the early days of use for every woman. After the first year of Depo (depending on the age and weight of the woman) about a third of women will have no more bleeding.
LW: What about headaches and depression?
Ask Jerilynn: It is not clear why headaches increase on Depo—they tend not to be serious migraine headaches but are more stress type. Perhaps they are related to the higher stress hormones the body makes whenever estrogen levels drop. Unfortunately, headaches tend to increase over time, rather than getting better as the not-so-funny bleeding does.
The reasons for depression are mysterious to me but this is an important adverse effect. I believe that anyone who has previously had an episode of depression (whether diagnosed or not, but sufficient to interfere with life and work) should avoid Depo.
LW: Although there has been little discussion about bone health concerns on the previous blog post, I think we should address the fact that Depo causes bone loss. How does it do this?
Ask Jerilynn: As we discussed, Depo causes estrogen levels to drop. Dropping estrogen levels always cause bone loss. Several randomized, blinded studies for example, have shown that if women taking Depo wear an estrogen patch, compared with a placebo patch, they don’t lose bone. (That was a test of the cause of bone loss but isn’t a good strategy during Depo because it might prevent its contraceptive effectiveness).
The bone loss concern is now decreased because we know that women, on average, regain all of that lost bone as they stop taking Depo. MPA, like progesterone, stimulates new bone to form but this formation is not visible while bone loss is high (as in, while taking Depo). The increase in bone density on stopping Depo is because rising estrogen levels prevent bone loss and the increased bone formation then becomes visible.
I have tended to think the bone loss is not an important problem because the bone density returns to normal. However, women at osteoporosis risk do have more broken bones while on Depo. Therefore I recommend that all woman choosing Depo for contraception have at least three high calcium (dairy or calcium-fortified) foods per day (or take one 500 mg calcium pill with a meal and the other at bedtime) plus also 2000 IU of vitamin D3 daily.
It is probably wise for teens to avoid Depo if they have a personal history of amenorrhea (no flow for three or more months), or a close relative (mother, grandfather or sister) who had a broken bone without a major fall. (Note: For more life cycle specific information about preventing bone loss click here.)
LW: Weight gain has caused grief for many women taking Depo. What’s going on?
Ask Jerilynn: The suppression of women’s estrogen production likely causes the weight gain on Depo (that averages 2 kg or five pounds in the first year). A similar weight gain occurs in women or in animals when their ovaries are removed. It is probably the body’s way of trying to increase fat (that can convert male and stress hormones into estrogen) and thus to prevent the rapid bone loss that happens when estrogen levels drop.
LW: Another reported effect of Depo is digestive problems. I’ve read that abdominal distress including cramps, bloating and constipation are common because Depo loosens the tone of the muscles in the gastrointestinal tract. Can you comment on this?
Ask Jerilynn: I don’t really understand this. What I do know is that abdominal problems are common in general for women and haven’t shown up as significantly different between women on Depo or placebo in trials of Depo. I suspect, again, that the drop in estrogen level triggers stress hormones that cause crampy gut pain and changes in bowel habits.
2) Stopping Depo-Provera: What is causing adverse effects and what to do about them
LW: Thanks for explaining the side effects women experience while taking Depo. What happens and why are women miserable when they stop it?
Ask Jerilynn: First let me say that I have looked in the recent medical literature and been unable to find any studies of women’s experiences on stopping Depo. One would surely hope that drug regulatory bodies have required research on the return to fertility in women taking Depo.
Here’s what I think is happening, and I’ve formed this understanding based on what women described in their posts: Women’s reproduction has been suppressed by Depo for months or years. This means that (figuratively speaking) the hypothalamus, pituitary and ovaries have ‘forgotten how’ to coordinate their usual complex and amazing feedback needed for normal ovulatory menstrual cycles.
However, our bodies are programmed to work hard to regain reproduction so there is a kind of rebound over-stimulation of estrogen levels (the easiest hormone to get the ovary to produce). The result is erratic but high estrogen levels causing nausea, sore breasts, fluid retention and abdominal bloating, mood swings and heavy or prolonged vaginal bleeding.
With high estrogen levels and weight gain, plus the “hypothalamic incoordination,” ovulation doesn’t occur and therefore no progesterone is produced. Progesterone – the hormone produced after ovulation in normal menstrual cycles – is needed to counterbalance the high estrogen levels. I believe that it is this estrogen-progesterone imbalance that is leading to all these miserable symptoms.
LW: Many women who have shared their experiences on my previous post also seem very concerned by the delayed return to normal menstrual cycles, with some experiencing no bleeding for months. Others seem to have flooding and continual flow. What’s up?
Ask Jerilynn: We’d have to study this to be sure, but I suspect that the women who have no flow for months on stopping Depo likely are younger, have gained the least weight and are under the most situational/emotional/physical stress. On the other hand, those who have heavy and/or prolonged vaginal bleeding are likely older (and often perimenopausal—when ovarian hypothalamic coordination has normally become dysfunctional) and have usually gained more weight.
Therefore I believe that the varying responses in vaginal bleeding depend on whether women were on the young-thin-stressed side when starting and stopping Depo versus normal to now overweight or obese. Another possibility is that women have become perimenopausal during their years on Depo. Thus when they stop Depo they are now in a symptomatic perimenopause that the Depo was preventing or treating.
LW: Some women have noted extreme weight gain upon stopping Depo. Can you explain why this might be happening?
Ask Jerilynn: If estrogen levels are high and progesterone levels are low, the natural result is inappropriate hunger and weight gain. Progesterone levels following ovulation make women burn about 300 more calories a day, which obviously helps prevent weight gain. I think this weight gain side-effect of stopping is also due “estrogen dominance.”
LW: Another common experience that disturbs women as they stop taking Depo-Provera is extremely sore breasts. What causes this?
Ask Jerilynn: This is directly caused by the “estrogen overdrive” as the body tries to recover from the suppression caused by Depo. Sore breasts tell us that our estrogen levels are higher than the highest normal mid-cycle estrogen peak. If it is sore when you press your palm onto your nipple, you don’t need a blood/urine/saliva test to know your own estrogen is higher than it ever should be in the normal cycle.
LW: Why are some women getting acne or pimples on their face and backs?
Ask Jerilynn: Whenever women are overweight and not making enough progesterone (because they are not ovulating) the body makes more male hormones that lead to oily skin and acne.
LW: What about the hot flushes that some women are experiencing? These symptoms are typically associated with perimenopause, the transition to menopause.
Ask Jerilynn: Yes. Some women who have become perimenopausal while on Depo will have had their hot flushes and night sweats effectively treated by the progestin. Therefore, when they stop, they experience the symptoms of perimenopause including night sweats and daytime hot flushes.
That brings me to another educated guess—many women stop Depo in their 30s and 40s because they want to have a family or because their doctors advise them to. They may already be starting into perimenopause but the signs, such as hot flushes, are masked while on Depo. However, off Depo the estrogen swings (that may be high both because of stopping Depo and because of changes related to perimenopause) cause hot flushes and night sweats. If you’d like more information about perimenopause here’s a recent open-access scientific review.
Heavy flow is one of the most common experiences of early perimenopause that at least a quarter of all women experience. When you add the estrogen excess production on stopping Depo to perimenopause (“Estrogen’s Storm Season”) you get really, REALLY heavy flow. No wonder women are so frustrated and doctors are so puzzled.
LW: Many women are told to just “wait it out.” This could mean months of not ovulating, ages without a menstrual period, or putting up with flooding menstruation. Do you think that’s a good idea? If not, what would you suggest?
Ask Jerilynn: Based on what I’m guessing is going on hormonally, and also on a woman’s age, her desire or not for pregnancy, and on her current body mass index, here are some suggestions:
Heavy vaginal bleeding: My first suggestion—something every woman should know— is ibuprofen. One tablet four times on every heavy-flow day, decreases flow by almost a half. See this article about how to manage flooding or heavy vaginal bleeding. You can take ibuprofen on your own and track your own cycles by downloading and completing the Daily Perimenopause Diary.
Having such a record will help your health care provider to understand what you are experiencing as well as allowing you to know for yourself what is going on. If ibuprofen does not sufficiently decrease heavy flow so you can cope, you will likely need to ask your physician’s help. You will need a prescription in order to take what I next recommend, cyclic or daily progesterone. What works best is to print out this information sheet for on Cyclic Progesterone Therapy, one for yourself to stick somewhere obvious and one to take to your doctor.
However, if your flow has been so heavy and long that you already have iron loss anemia (commonly called a “low blood count”), have had continuous flow for over a month, or are bleeding enough to become dizzy when standing, you need a more powerful solution than cyclic progesterone. The answer is progesterone every day for three months (plus ibuprofen on every heavy flow day). I’ve written this article on heavy flow to take to your family doctor.
No flow for three months after stopping Depo: I suggest starting to take natural, bio-identical progesterone (see Cyclic Progesterone Therapy) for two weeks and stop for two weeks. Don’t be discouraged if you don’t get a period when you stop it. Just keep doing that two weeks “on” and two weeks “off” progesterone until your flow returns. Even without flow, this treatment will increase bone density (based on a trial we did years ago).
If, in the course of taking cyclic progesterone you start getting irregular flow, follow the instructions (and picture) in that handout carefully. Most of all, think of this as restoring a normal balance of your own hormones and ovulatory menstrual cycles.
When you start noticing stretchy mucus about the middle of the month, this means your estrogen levels are recovering. Now you can actively start working on becoming pregnant, if this is your desire. You will take the progesterone for two weeks or fourteen days but start checking for your urinary LH peak (with a fertility kit you can buy over the counter) in the evening when you notice stretchy vaginal mucus. Only begin the progesterone after you see the LH peak (a positive test) or after the stretchy mucus decreases. The reason is that if you take the progesterone too early it could suppress that necessary LH peak.
Sore breasts, bloating and/or nausea: These symptoms mean high estrogen levels, usually without any or enough progesterone. Increasing exercise, increasing vegetables and fruits, and decreasing junk/snacks and desserts (except fruit) will decrease estrogen levels in premenopausal women. Although I can’t promise that for women in perimenopause, it will certainly help you feel better. After you’ve started on these lifestyle changes, I’d suggest beginning cyclic progesterone 14 days after the start of a flow or any time if you are not getting flow regularly. Follow the suggestions about how to take progesterone on the Cyclic Progesterone Therapy. If sore breasts get better but still persist, you can also try (gradually) decreasing your caffeine and alcohol intakes.
Hot flushes and night sweats: To start, I think it is important to realize that the experience of hot flushes or night sweats means you are in perimenopause. So, although it is not much help, you can blame some of what you are experiencing on perimenopause instead of just on stopping Depo!
CeMCOR recently proved that progesterone is effective for treatment of menopausal hot flushes in a randomized, placebo-controlled trial. We are now testing its effectiveness for perimenopausal hot flushes in a similar controlled study. If you live anywhere in Canada, you could potentially participate.
If, as is typical in very early perimenopause, you are waking at night feeling hot (and often sweaty or irritable) on only a few nights a month, and usually around flow, then cyclic progesterone works. Take it for 14 days, but if you typically have night sweats on the first few nights of flow, continue it a few more days.
However, if hot flushes are coming day and night and are troublesome any old time, then take progesterone daily instead of cyclically.
LW: This information will certainly help the many women who are having these experiences. Is there anything else you want to add about Depo-Provera?
Ask Jerilynn: I would like to say, perhaps belatedly, that Depo is an effective contraceptive that I feel women should have the option to choose. (Here I may differ from Laura!) Those of you who know me (and CeMCOR) realize that my goal in life is to help every woman achieve normal, ovulatory menstrual cycles. However, not every woman is — because of living conditions, partner attitudes or general life chaos — to manage barrier birth control methods that support ovulatory cycles. For women who should not take estrogen-based hormonal birth control (past blood clot, liver problems, heart problems, severe migraines, smoking, or over age 35) Depo may be an effective and valued contraceptive. Here’s a quote from one post, “I too was on the depo, for 11 years actually during this time I loved it…no periods, no PMS awesome. . . .”
LW: Point taken. I agree women should have access to Depo-Provera for the reasons you mention. But, what that commenter wrote next was: “My god what happened post depo I never ever thought I would go through…throbbing sore breasts to the point I couldn’t even touch them, night sweats (a year) anxiety, major bloating, nausea, withdrawal from social events, weight gain mid section and boobs…I hated life!!!!” I think this is the “nightmare” scenario I was referring to in the title of last April’s post. Let’s hope your suggestions above are helpful for her and everyone who has commented, or will comment, on last year’s post.
What I find unacceptable is the lack of information women have about how this drug works and what its effects are both during and after use, as well as the lack of assistance available from healthcare providers in recovering from the drug. Thank you so much for explaining some of what is going on for the women who’ve been sharing their experiences here at re:Cycling, and for offering suggestions to help in their recovery from Depo-Provera.
Note to readers: Please feel free to share the PDF document of this interview with other women and health-care professionals who may find the content of value.

I am so glad to see this discussion online. I think there is not near enough research that established clearly the endocrinological response to coming off of contraceptive endocrine disruptors (CEDs), like Depo-Provera and its kin. So much right now is reasonable conjecture and anecdotal, which is of value but not conclusive or universal. I am of the mind that if we do not know well the full implications of a drug (CED)both starting, using, and stopping we should probably not be using it.
There are many factors to consider with respect to how a woman will respond to CEDs, which include general health status, diet, lifestyle, stress, chronic illness, genetic predisposition for endocrinological disturbances, liver health, gut health, emotional health (which is related to all of the above), among other factors.
Another cause of acne can be the conversion of progesterone into dihyrotestosterone (DHT) in response to elevated cortisol levels.
My osteoporosis support group members laughed at the absurdity of asking a women chosing depo (quite likely because she didnt want to take a daily birth control pill) to now take 3 pills per day (calcium + 2 Vit D)to ward off bone loss.
A patient in the pharmacy where I work had digestive disorders and annovulation for 2 years post depo; she could not afford supplements and was forced to rely on drug treatments for her symptoms that were covered by the province. Being one of the thin, young, stressed variety Jerilynn describes, she is now sickly with malabsorption issues which increase her risk of osteoporosis and other chronic conditions.
I agree that she has the right to choose depo, but in my opinion, public health nurses have work to do in the informed consent department when reviewing the birth control options. I understand that their job is to reduce unplanned pregnancies and depo is cheap, but at what cost to the individual and ultimately to the health care system burdened with treating side effects and managing long term risk?
Absolutely Lisa. Informed consent is so important. And it is valid to ask how then is women’s health recovery supported after having suffered the ill effects of contraceptive endocrine disruptors.
Lisa , how long was that patient on the depo and what was her digestive problems? I took the shot once and continue to have stomach trouble
I totally agree with you, Lisa. And it’s not just public health nurses. As far as I’m concerned any sexual health clinic care provider, gynecologist or general practitioner who is willing to prescribe this drug better be willing and able to counsel and support women coming off this drug. I believe that if women were given the kind of information included in this post, many fewer of them would agree to take this drug.
I also scoff at the irony of telling women who chose Depo because they can’t remember to take a pill everyday that they must take calcium 2 to 3 times a day plus vitamin D.
The patient I described had 2 or 3 shots of depo and digestive issues (IBS symptoms with pain, specifically)for a good 3 years post depo, but she’s lost to follow up, unfortunately.
btw – I recommend probiotics for IBS. Favorite study supporting this is A Controlled 6-Month Intervention
by K. Kajander et al(Aliment Pharmacol Ther. 2005;22(5):387-394.) Showed steady improvement over the 6 months of the clinical trial on all measures of IBS with probiotics over placebo.
We know that oral contraceptives can disrupt gut flora (discussed briefly in “Coming off the Pill” by Lalonde and Matus), and many other dietary factors contribute to dysbiosis, as does antibiotic use. So intestinal illnesses are prevalent in many pops and play a role in various health matters from obesity to cholesterol, immunity, and so on. Point is – there’s often more than one factor at play in health and illness which is why we need to treat patients as individuals rather than a herd.
Thanks so much for posting this discussion, Laura. We will link to the Depo documents on our CWHN website.
Thank you Lisa
I agree thank you
Also Lisa do you have an email address I have a quck question or if you can email me erickawebb26@yahoo.com
Hello Anne -We were fellow members of the Toronto Women’s Health Network in the early 90’s, and I remember you and colleagues being very concerned about Depo Provera back then.
I was dubbed “the mucus lady” after I gave the group a Justisse Method intro one meeting.
Lisa Leger, now of Vancouver Island and still teaching FAM.
Hi Lisa
Definitely remember you! Send an e-mail address to ed@cwhn.ca so we don’t continue to clutter Laura’s space!
Anne
Hi,
I’m only 21 I took the depo once in September 2012 and from the beginning of October I have been bleeding it differs from heavy and light this is really getting to me now
I have read the interview above and I’m a little bit worried as I am starting to get hot flushes as night and it says that’s a sign of perimenopause, but how can that be I’m only 21 does this me I will not be able to have children in the future
I just wanted to leave some positive comments about Depo. My whole life I’ve had horrible periods. 10-12 hours of cramps so bad I couldn’t get off the bathroom floor, and flow so heavy I couldn’t leave the bathroom anyway. The pain was so bad that I remember being 16 and in between screams of pain begging God to just kill me now. I’ve even had apartment neighbors call the police because they thought someone was attacking me. I tried the pill but couldn’t remember to take it regularly, so periods never stopped. I tried to get my OB/GYN to pull everything out because I don’t want kids anyway, but being told “oh, you’ll change your mind”. When I turned 31 I decided I was fed up and went on Depo. Bone density loss didn’t concern me, because I was already taking a calcium/vitamin D supplement (I’m white and skinny, 5’7″ and 120 lbs when I started Depo) and obviously the possibility of gaining a few pounds didn’t bother me. I’m now 34 and have been on Depo for 2.5 years. I ended up gaining 25 lbs (mainly because I’m not as active as I was since I’m now caregiver for my granddad and not walking around all day at work in a vet clinic) and have not had a period (and the dreaded cramps) since the first shot. I have a little discomfort right after the shot is given, but that’s to be expected with any IM shot. Other than the weight gain, nothing. I can tell when its getting close to shot time because a little of my PMS irritability peeks through, but no bloating, no anemia, no cramps, no breast tenderness, nothing. My only complaint is that with all the weight I gained, none of it went to my horribly small boobs. I plan on staying on Depo until they either let me get a full hysterectomy or I hit menopause. Maybe then the doctors will realize I really didn’t want kids 🙂
Here is a reply from Dr. Prior:
Hi Charelle,
Let’s see if I understand. You took Depo-Provera only once in September 2012 (and it should last for 3 months). But in October while the drug was still “working” you started getting heavy or light flow but most of the time and you started having night sweats? Is that right?
About the flow: On heavy flow days take an ibuprofen or other over-the-counter “Nonsteroidal anti-inflammatory medication” to help decrease the heaviness of flow.
About the night sweats: I’m sorry for worrying you about the night sweats. What I meant to say is that usually a woman who gets night sweats when stopping Depo is going into perimenopause. However, sometime, although rarely women will get them after a pregnancy and still be able to go on and have other children. So don’t worry on that score.
But it is unusual to have hot flushes or night sweats while the Depo is still in your system.
The only things I can suggest are:
Keep the Daily Perimenopause Diary (that one only because it allows you to record night sweats or hot flushes) to give yourself and your doctor a record of your experiences. Here’s where you can find the Diary and instructions for recording. There are also some YouTube videos. . . . https://www.cemcor.ubc.ca/files/uploads/daily_perimenopause_diary.pdf
Take ibuprofen every six hours while awake on heavy flow days. Try not to worry about the future but just cope right now while continuing to eat well, get good sleep and exercise regularly.
I’d be interested to know how this plays out. I suspect that all of this unwanted stuff will soon go away. . . Let’s hope!
Hope this is helpful for you,
All the best,
Jerilynn
Thanks for commenting. Certainly this contraceptive choice works well for some women and I appreciate your taking the time to share your story. You make a good point about not being trusted to know your own mind as regards your wishes to not have children. I wish you well in the future.
Thank you so much for this article I swapped from Depo to transdermal patches in January, after being on Depo for 3 years. I am experiencing many of the symptoms you describe, to the extent I took a pregnancy test last week thinking the patches must have failed me! I have very swollen and sore breasts, I am bloated and have put on 10lb in weight, and am suffering with significant anxiety, stress and mood swings, as well as headaches. I am comforted by the similar stories of others and now feel comfortable in just waiting for this to pass, as I’m sure it will. I did feel that there were many benefits to Depo, having also been on it for several years when I was younger, and I think there just needs to be more widely available information about the potential for these after effects.
Hi
I started taking the depo after my 3 child, I was 31. When asking about contraceptive I wanted to make sure I had no more kids, and the depo sounded perfect. I had some spot bleeding not much, now and again, sore breast a few times, but life without periods was great. Just before christmas i went for my normal 12wks injection and the nurse, ask if i had thought of coming of the depo. I said no, as i couldnt think of anything worse my periods returning or worse having another child. She then explained about my bones, which i knew nothing about. I have been on this depo for 10yrs, Im now 42 i have’nt taken any Calcium or Vit C. It has been 5month since i came of the depo. I had sore breast after 2mths for about 8 days i couldnt take my bra of as the pain was so bad. I have had stomach cramps for the past 2 days, and now feel very low. How do I know if this has caused any damage to my bones? are there any tests I can have? Should I start taking the Vit D and Calcium now? Im 42 and and worried i cant repair any damage done in time. Any advise would be great?
Reply to Karen re bone density worries:
The most well accepted standard test for bone density is called the DEXA. Its a very low amnt of xray and it compares your score to a healthy young person. There is also a risk assesment tool called FRAC here: https://www.nof.org/articles/8 that is highly thought of in the medical community, since bone density alone is just one risk factor. As for Depo, the party line from the ob/gyn community is basically “dont worry, you can gain bone density back once you quit depo.” however they looked briefly at younger women to determine this. Finally, supplementation is gen’ly endorsed by most agencies, but recent findings have caused some to reduce the dosing recommendations on calcium to 1200mg per day total (incl that acquired from food). http://www.osteoporosis.ca has a calcium counter that helps you figure out how much you get from food so you can calculate how much to supplement. The benefits of Vit D are piling up and Osteoporosis Canada recommends 800-2,000IU per day. Doctors can test your levels and recommend higher if deficiency is detected.
opps – sorry its FRAX, not FRAC
(just checking for typos…)
Hi there,
This interview was very interesting to read, thank you for posting it. I thought I’d share my experience in the spirit of having more informational comments to help people (and myself!) understand this drug, which I plan to be on for a couple years if I can handle it.
I’m 24 and got my first shot May 9 2013 on the 4th day of my period because of a strong desire for hassle-free protection following a pregnancy scare. Initially, I had a very odd reaction to the injection; about 15 second later, I felt like I was going to faint…felt really woozy, but the feeling went away after an hour or so, then I felt fine.
For the past couple weeks I’ve been waiting for the side effects of being on the shot to begin, convinced they will, because I had awful side effects on the minipill a few years ago (heavy prolonged bleeding, nausea, weight gain, depression, etc) and I already suffer from emotional, digestive, and autoimmune disorders. I’m so used to constantly feeling crappy, taking a bunch of daily meds, that I like to be as informed a patient as I can be, so you can see how all these Internet comments have terrified me about what I could be in for!
So far, I have had no side effects at all (that I can’t attribute to my other meds/disorders) except very, very light spotting starting today (about 2 weeks post shot). No weight gain problems yet…I am 5’7″ with a very thin/toned figure and fluctuate between 138 and 144lbs depending on where in my cycle I am, and my weight has stabilized around 137-138 the past 2 weeks (yay!) My boobs don’t hurt, my libido is the same, and I’ve had no [extraneous] emotional/mood problems, no acne, no hot flashes, etc.
I’m very aware that I can probably expect the above side effects to begin shortly, but I’m hoping if I keep a positive attitude (or at least try to…) I’ll be spared the agony for now due to my age, timing of first shot (does that even matter?) and relative good physical health (have been taking vitamin D, calcium, iron, and probiotic supplements regulalrly for years and have terrific blood test results).
When it’s time for me to come off the shot, I plan to do so in a way that will cause the least problems. I can’t expect any help from the clinician who gave it to me – she didn’t even bother offering up any info about this drug unless I asked! So, any further guidance you could suggest given my provided history would be appreciated.
Thanks again for the info! 🙂
-Kelly from Pennsylvania
most positive thing I can say to Kelly is “keep using the probiotics”. they are your best friends, those friendly little flora, and have recently been shown to down-regulate an overactive immune system that’s misbehaving.
now for a bit more negative comment: when a patient already has auto-immune and digestive issues, we shd be talking about ways to remove straws from the camel’s back rather than adding to the toxic burden. Just suggesting that someone who is already not well, should not be offered more to carry or eliminate, but rather be invited to lighten their load before the last straw is reached.
When stopping Depo or other hormonal contraceptives there are some helpful thing to know. I suggest that you read “Coming Off the Pill, the Patch, and other Hormonal Contraceptives” written by Megan Lalonde and myself. https://www.justisse.ca/ComingOffThePill Additionally, the information contained in this small guide is important for overall health and reproductive health.
Many of the symptoms for which women are prescribed hormonal contraceptives can be alleviated and actually cured through attending to some diet and lifestyle changes. Hope this helps.
1 I am not premenopausal i am a soldier I am 25 very active and healthy. I’ve been on depo since jan 12 got off feb 13. I’ve had heavy bleeding every 2 weeks tender breasts been cramping moody and I’ve put on 5 pounds since stopping that just won’t go away. I didn’t have any of this before my daughter and I worked my butt off to lose my pregnancy weight to gain 5 pounds and a heavy period after stopping depo so what’s up with that?
And I also can’t sleep cuz I wake up hot and sweating even though my house I extremely cold at night
I was on the Depo shot for 12 years. I am now 31 and didnt
start my period for 10 months after stopping the injections.
I now have irregular periods that last for 2-3 weeks with heavy flows with abdominal cramps and nausea. Just wanted to
know if this will go away on its own or do I need to see a
Doctor for treatment as I do not have insurance right now.
I am also seriously thinking of going back on the Depo because I cant stand the horrible cramps and heavy flow. Any advice would be much appreciated.
Hi Heather – When you think about it, a doctor’s “treatment’ will likley consist of more hormonal interventions. I’d recommend Not getting more synthetic hormones in your system, since that is what caused the problems in the first place. Instead, consider seeing a Naturopathic Physician and get your cycles back in order using nutrition and natural remedies. It can definitely be done and you will be healthier overall. If you can’t afford a ND, then look for a Justisse HRHP at http://www.justisse.ca We do consults in person and online. You can also get some suggestions at your local health food store if they have someone on staff who know about women’s health.
I’ve been on Depo for almost a year. I’m 26, 115lbs. My mother had breast cancer, my grandfather passed from multiple cancers. I understand there hasn’t been any scientific proof of Depo being linked to breast cancer, I have read many conflicting articles about Depo and the hint (just a hint) that B cancer may be linked. Using words like hint and may don’t make me feel confident. Im going to discontinue using Depo and I’m quite afraid of this process, reading more into Depo other than what the doctor told me I am now finding that my low libido, hair loss (i have lots of thick hair thankfully but there is a huge amount that comes out with every shower/hair brushing), depression and lack of confidence in myself not only physically but mentally, quick to anger and acne not only on the face but on my head, back and chest (yep yuck!) can be a result of the shot. And don’t forget the lingering possibility of Breast Cancer..I wasn’t aware that this shot makes your body think its pregnant constantly, I started having relationship problems and decided to do some more research about Depo and the side effects your doctor may have skimmed through. This is a horrible birth control option it sounds like for MOST women, I do see some positive feedback but these cases seem rare. I’m angry that I ever accepted Depo into my body and now I’m angry to have to wean myself off. Is it heroin we’re talking about or birth control? I’m not looking forward to next few months of getting Depo out of my system and finding a new birth control that isn’t made by corporate America. But I do appreciate this site and the information. Life could be worse but good luck if you think Depo is the bees knees.
Thanks for the reply, Lisa. You’re absolutely right – with so many problems I shouldn’t add even more toxic properties to my body, but I do need a reliable form of birth control at this point in my life, in my current relationship. However, I’ve been taking lots of good probiotics and seem to be doing well in all aspects. Aside from some extra bleeding that is so light it doesn’t get in the way of anything, I still haven’t experienced anything negative on Depo. I’ve even lost weight! But I know based on others’ reports I can’t expect this to continue, and my doctor suggested I go on Skyla in July when this first shot is up. I need to do some research about the switch between the two hormones, and I’m nervous about how my body will react. I guess we’ll see. Staying optimistic is important, I believe!
As we see here in this comment section there are women who experience Depo-Provera as a helpful aid to their menstrual cycle difficulties and concerns about avoiding pregnancy and others who experience the drug as devastating and not worth its birth control properties. What I invite readers to consider is the fact that Depo-Provera is a drug that profoundly disrupts a woman’s endocrine system in order to make her infertile. Considering the ways in which our endocrine system interfaces with our immune system, neurological system and every other body system it is short-sighted to think that we can use this drug without serious health consequences–despite the scientific rhetoric. Also, there are much more healthful ways to address menstrual cycle difficulties through diet and lifestyle and nutritional supplementation, approaches rarely ever addressed in mainstream medicine. I invite women to seek these approaches first. Try reading Alexandra Pope’s “Wild Genie” or the multitude of other approaches for healing PMS naturally and addressing issues such as heavy bleeding and painful periods. My clinical experience since 1977, attests to the validity of these approaches.
Do you recommend a particular probiotic? I prefer natural.. but not sure if there would be enough in foods. Long story short, after much research and diet changes.. apparently 9 yrs on depo completely ruined my digestive system. I have been through many tests- so no, it is not colitis, celiac’s or anything else. I recently switched to whole foods, clean, non-gmo, vegan, gluten-free, sugar-free in an attempt to not be devastatingly sick. I *just* stopped the shot (I know, it took way too long to discover the real problem but NO medical professional would even consider the link.) I’m trying not to be utterly depressed over this, as I wonder if I will ever return to some kind of normalcy. But I would love any recommendation on probiotics, thank you.
With respect to probiotics for a ‘messed up gut’ I would suggest that the person with the difficulty seek a clear diagnosis of what is causing the dysbiosis so that they can then choose the most beneficial probiotic and/or antimicrobial remedies. They might start with a comprehensive stool analysis through a lab such as Genova Diagnostics http://www.gdx.net where they will identify what is messing up the gut and then recommend the appropriate remedies. Also when a gut is messed up there is a chance that food sensitivities allergies enter the picture. Here again proper diagnosis is helpful. Check out Meridian Valley Labs ELISA food allergy testing https://meridianvalleylab.com . The health of the gut is an extremely complex thing and gut health affects mood, immune function, and endocrine function. So it is worthwhile attending to but complicated and getting sound advice and diagnosis from a qualified practitioner is advised.
Thank you for all this helpful information! I’ve had a similar experience to other commenters. Loved depo for two years, no unwanted side effects like with oral contraceptives. About four weeks after what should have been my next injection (which I purposefully opted out of) I was convinced I was pregnant, experiencing extremely sore breasts, weight gain in breasts and midsection, lightheadedness, hot flashes…the list goes on. Flow returned, pregnancy tests negative, and symptoms persist. I’m 22 and in excellent health. I’m quite physically active and I make healthy eating a major priority, especially due to the fact that I’m gluten intolerant. I was curious if, besides progestin, there is anything more holistic I can do to improve my situation. I’m wary of messing with my system, and I already lead a healthy lifestyle. I understand that it takes time for one’s body to recover from this, but if anyone has any advice I’m welcome to it. These past three months have been completely miserable and adversely affecting my quality of life! Again, thanks for all the great information!
I thank God i found this website.I have a question to the dr or Lisa. I gave birth on jan/2013 i took my first dose of depo Feb/2013 i started spotting, gaining weight mild cramps by may prior to the scheduled date for my 2nd dose i started having pregnancy symptoms. I hated depo so i decided to discontinue never got 2nd dose. On the last week of may ( my 2nd shot was scheduled) i started bleeding as i normally do on my period ( heavy) this lasted maybe 3-4 weeks so we can say i had a period between may and june. I felt i was going back to normal in june i even lost a couple of pounds and didnt get on any birth control either. On july i didnt have a period and the symptoms i had while being on depo started to intensify i took 2 pregnancy tests came out negative ( i also took one the last week of may and it was also negative) i had a drs appointment on august/2 dr wanted me to take another test and it came out negative i gained more weight and she told me to be on the pill to regulate period. Ive been on the pill since aug/3rd/2013. Ive been feeling the same symptoms described above ( cramps, nauseas, tender breasts…i feel pregnant) they come and go and noo symptoms of period either. MY question is should i continue with birth control pills? is it going to help me or is this going to make the process of going back to normal to be longer? I told my dr all these symptoms and she seemed like she either didnt care or she knew it and didnt wanna tell me. She never warned meb of all these side effects ONLY about bone loss and she said that i go through that when pregnant and worse kinda saying you better off with the shot than pregnant anyway. This is so upsetting. I do not want to be pregnant this year ( i had a c-sections) but would love to try for another baby at the end of next year. Another question is does depo alter a pregnancy test? i kee getting negative results but they havent been blood test, my dr told me no but now i do not know what to believe anymore.
THank YOU soo much.!!!
I thank God i found this website.I have a question to the dr or Lisa. I gave birth on jan/2013 i took my first dose of depo Feb/2013 i started spotting, gaining weight mild cramps by may prior to the scheduled date for my 2nd dose i started having pregnancy symptoms. I hated depo so i decided to discontinue never got 2nd dose. On the last week of may ( my 2nd shot was scheduled) i started bleeding as i normally do on my period ( heavy) this lasted maybe 3-4 weeks so we can say i had a period between may and june. I felt i was going back to normal in june i even lost a couple of pounds and didnt get on any birth control either. On july i didnt have a period and the symptoms i had while being on depo started to intensify i took 2 pregnancy tests came out negative ( i also took one the last week of may and it was also negative) i had a drs appointment on august/2 dr wanted me to take another test and it came out negative i gained more weight and she told me to be on the pill to regulate period. Ive been on the pill since aug/3rd/2013. Ive been feeling the same symptoms described above ( cramps, nauseas, tender breasts…i feel pregnant) they come and go and noo symptoms of period either. MY question is should i continue with birth control pills? is it going to help me or is this going to make the process of going back to normal to be longer? I told my dr all these symptoms and she seemed like she either didnt care or she knew it and didnt wanna tell me. She never warned meb of all these side effects ONLY about bone loss and she said that i go through that when pregnant and worse kinda saying you better off with the shot than pregnant anyway. This is so upsetting. I do not want to be pregnant this year ( i had a c-sections) but would love to try for another baby at the end of next year. Another question is does depo alter a pregnancy test? i kee getting negative results but they havent been blood test, my dr told me no but now i do not know what to believe anymore. anpter thing im 29 years old.
THank YOU soo much.!!!
Yes, the hormonal contraception will likely make the process longer of getting back to normal.
Depo shouldn’t alter a pregnancy test, as they test for HCG, which is a hormone that would show up if you were pregnant.
You may want to try learning the sympto-thermal method of fertility awareness and use condoms temporarily, if they work for you.
ugh – I am So Sick of doctors telling women that the pill will “regulate their cycles”! Any fool can plainly see that the pill cant possibly Regulate the menstrual cycle because it’s whole mode of action is to Suppress the menstrual cycle in the first place. All its regulating is when the patient can expect to see the withdrawl bleed that is a function of not using the synthetic hormones for that week.
It is inconceivable to me how a doctor could misrepresent the pill as a treatment for irregular cycles, since it does nothing therapeutic to correct the underlying problem whatsoever. Is that even legal or ethical? Its like putting someone on a respirator instead of figuring out what they’re allergic to or giving powerful daily pain meds instead of identifying headache triggers.
In fact, lets quit calling that fake bleed between pill packs a period all together. grrrh
I took one shot last year in Aug. so as of the day its been a year since my one and only shot. I had the worst time for the 3 months and once the shot “ran out” I started having stomach problems after a lot of test and blood work I was told my gallbladder is functioning border line low. I had no idea that birth control can cause gallbladder problems. I’m not going to have the surgery to have it removed because that will bring on other problems. Has anyone else had this problem or stomach issues in general after taking the shot?
Gall bladder is listed in the warnings that come with hormonal contraceptives. I work in a pharmacy and have been taking an informal poll. When women tell me about their digestive or gall bladder issues; I’m finding that the majority did in fact use the pill in their past.
Also, my daughter yakked almost every morning when on the pill and had abdominal pain (along with moodiness and puffiness). All this went away when she quit and shes a healthy happy woman again.
Hi – your questions were about whether to take the pill or not, and its no surprise that I’d suggest not.
From the perspective of a holistic reproductive health educator, we want you to have your normal healthy cycles all the time and especially when you’re planning another pregnancy. You might be more comfortable with quitting if you knew there is a effective natural alternative; fertility awareness methods can be used to avoid pregnancy and also serves as a health record and diagnosic tool in case your fertility does not return on its own. Meanwhile, the good old condoms can cover off those days when you are not sure about your fertilty status. Visit http://www.justisse.ca for details on charting and there is a list of teachers there as well so you can arrange a consultation via skype, phone or email.
Lisa 1st off thank you for responding. I still have stomach muscle cramping and weird pains at times. I can say at times passes they don’t come as much. Is there anything you can suggest for the gallbladder because I don’t think I should have this removed just from taking one shot a year ago. Also from your experience and study how long does this crap linger in the body because it different than the pill
Huh. My gallbladder stopped working and I had to have it removed. I was on the shot at the time. Since I was on the shot, my digestive system has been an utter mess. I have a long list of food intolerances now. How come, with my five thousand visits to numerous doctors, not one of them made that connection? Nice system we have.
Nicole how long did you use the shot and are you still on it now? Did you have gallstones/ and how is your body now that you have had it removed? did you gain weight and I have read that once removed you use the restroom after every meal
Thank you sooo much!!!!!! 🙂
My last shot was four months ago. It has been one month off. Basically I was on it for almost 9yrs. And with my five thousand issues.. the shot is the only common denominator. I didn’t have stones.. just a gallbadder that stopped functioning. 0% The first couple of months were *horrible* but I have learned so much since that it could have been so much easier. I was def rushing to the bathroom after every meal.. or during. But there are digestive enzymes or even gallbladder bile that you can take.. which, of course the doctors don’t mention. I found that out on my own. Without giving too much info.. I suffered from severe diarrhea for years and years.. however it turns out I am lactose intolerant and gluten intolerant to boot. I finally started probiotics and things are so much better (of course cutting out dairy and gluten did wonders). I have to wonder though if I could have reversed the damage to my gallbladder through diet alone. I would definitely research that first before having yours removed. I wish I had. Mostly not having a gallbladder is no big deal but I’d rather have all my organs. But the shot has definitely screwed my entire body up big time and I pray I can reverse that….
Nicole do you mind emailing me for a short side bar conversation I just wanted to go over some info
erickawebb26@yahoo.com sorry to bother you but the info you have seems helpful for me thank you and God Bless
Hi all,
I am absolutely shocked reading this article and the following comments.
I am from the UK, and when I was as young as 13 I was advised due to severe PCOS that chance of me having children was slim to none but to combat the effects of the heavy periods and pain the doc suggested the shot – not the pill ( as I have a horrible family history of diabetes, obesity, heart troubles etc).
I took a year and and a half worth of shots and the bonus was no period! I stopped taking the shot as, like all teens, I was told I couldn’t have kids anyway and I wasn’t getting periods so I stopped going, and I became sexually active, obviously too young and at 16 fell pregnant with my only child. Straight after this I was on the mini pill for 6 weeks as I was breastfeeding and then back to the shot.
The shot I have taken intermittently for now 8 years. I’ll have a few shots on time, miss one by a few weeks or a couple of months and then back on it. I didn’t think I had any side effects.
However, after reading this article I realise I had most of them. Over the past year I have found myself extremetly irritable, hostile, self concious, paranoid, I have found an extreme dislike for the company of others, to the point I stay in the house for days. My hair falls out, I am bloated and several months ago, after 8 months of agony, I was diagnosed with a massive sack of gallstones in my gallbladder – and my GB was infected and inflamed, I needed hospitalised and then emergent surgery to remove the GB as my diet is a good one. Now I suffer from ‘Bile salt intolerance’ and my diet is very very limited and I suffer chronic Diarrhea.
I’ve been reading up on changing my method of contraception. I have a huge squeamish ‘thing’ about condoms’ so they are not an option for me, and I understand the feelings of synthetic hormones and contraceptives containing them but I have tried charting cycles previously and I never got it right – not only that, after years of continuous blood tests I am lucky to ovulate twice a year! I have the most heinous periods and am now undergoing treatment for cervical ‘issues’ we’ll just call them that. The docs wont remove the cysts as they say they aren’t dangerous but they dictate my whole reproductive ‘life’!
For those with GB issues – don’t get it removed if you can help it. Amend your diet, cut down on cholesterol, detox! I woke up with a tube in my stomach, and for all the stones may be gone, I’m left with the unfortunate situation where I can (and have), without warning and at any time, soil my own pants due to the urgency and severity of the Bile salt intolerance and chronic D. Please find another way!
Hello Jm do you mind emailing me please I wanted to get more info from you erickawebb26@yahoo.com
What is bile salt intolerance? I am unable to find any information about it.
It’s also known as bile salt diarrhea. It’s where the intestine fails to break down and absorb the extra salts from the extra bile now flushing through since there’s no GB. It causes urgency and yellow watery diarrhea. It’s a side effect in about 5% of people who’ve had gallbladder removal. It’s not commonly diagnosed as docs put it down to ibs quite often. But it entirely different and until they’ve done test to rule every single thing out. Which sometimes they don’t even bother to do. It’s not commonly diagnosed but quite an annoying and life changing complication. Can’t eat out. Can’t eat more than 5m from a toilet. Have to carry spare pant in me bag. Very embarrassing
I am 5 months since my last depo shot and have been constantly bleeding since my first injection 10 months ago.
I have been searching for answers on how to diminish the effects of depo since I started and recently decided to put together a survey (I am a statistician by trade, so I’m naturally curious anyway).
If you are currently taking depo or have stopped, please take 2 minutes to fill out my survey. I can share the results with you if you’d like, but I will NEVER ever use your information for anything other than calculating results.
https://www.surveygizmo.com/s3/1368485/Coming-off-Depo-Experience
Thanks! I hope this helps get some answers!
Hi ive been on depo for about 6 years and I am planning on not getting my next shot … My breast have decreased 2 cup sizes since I have been on it and have had joint problems. I am 21 now and wanting to have a kid soon with my husband although I am now scared that I want be able to have kids BC alot of my friends have gotten pregnant while on depo and I havent I need help and have many questions I have had irregular periods for the last 3 years after not having one for the first 3 that I was on it will someone help answer my questions I doNT want to end up having a body.tore up due to taking depo
Hi I took about two shots and then Had my last shot on December 2012 I didn’t get my period until August 2013 and have not stopped bleeding since I get dizzy out of nowhere. I get cramps. But what mainly bothers me is that I feel down and not myself for weeks,then i start feeling normal again and then few weeks later I’m back to feeling down. And same goes for my sex drive. I’m in a rollercoaster with my mood swings and sex drive. I told my obgyn doctor and they want to get me on the pills to stop my bleeding and get me feeling Normal again but I’m very bad at taking pills and I’m also afraid that when I stop taking them then ill be stuck with more symptoms. After reading your interview I was thinking if maybe there are natural pills that I can take to balance the estrogen and progestin or what you call it (not so good with doctor words) thank you much. Ps I looked up a her solution pill that helps make our hormones normal and Guelphs have normal periods every month and also help with sex drive. Have you heard of it and if so do you think this will help with all the symptoms thank you
*helps
Has anyone ever felt ovulation pain after stopping the depo I’m feeling pain on my left side of my pelvic just a pulsating dull pain also I’m feeling like throwing up i stopped my shot 3 months ago my period has come back normal . This weird pulsation pain is bothering me.
Missy, I had and still have the same pain, and for me it is not ovulation. For me it is just one of the dozen side effects of Depo which I am ‘waiting’ to end.
I am 30 now and I was due to have a follow up Depo shot in February 2013 (had 2 shots before that). Thank GOD I decided against it. I was experiencing a severe drop in sex drive, horrible mood swings, depression, and weight gain plus bloating leading up to February. It was not until this past July that I finally got a period, and it is now November and it has not stopped.
I wear a tampon everyday which is not only inconvenient but I know it can not be good for me. I have brown, thick bleeding with pieces of, what can only be, uterus lining in my ‘period’. I have suffered from night terrors and night sweats while on Depo and now while off of it. I feel my lower abdomen has swelled significantly. Also, I was a 34C bra size before I came off Depo. I bought a sports bra last week and had to buy a 34DD. My breasts are very big, extremely sore, hot, and hard to the point it is very painful to run (hence the new sports bra).
I feel my symptoms are no different than the other women on this site and the many other sites I have visited to try to understand why my body is reacting in this manner. And just like many women on this site, I was not informed by any health care professional that such negative reactions could occur. (I suffer from migraines and as a result turned to Depo as the pill seemed to make my migraines much worse during my early 20s)
I am a healthy active woman and I have always worked hard to stay in shape mentally and physically. A woman above mentioned that she questioned the difference between this and something like heroin in regards to the horrific side affects. I trusted my nurse and doctor when I made the decision to go on Depo, which I felt at the time was a well informed choice. I accept it was my decision, however I feel my health care provider should have informed me of the drug’s possible short term and long term side affects. I feel disgusted that I ever let anyone put this drug in my body. I want to have children in the next two years. Now I don’t even know if I have a chance due to the state my body is in, thanks to this drug. I feel like I am playing a waiting game but I’m not sure how long I will have to wait. What is worse, I can not seem to find any concrete answers on how long I will have to wait and what long-term damage I have caused my body. This is frightening.
I feel all of the women on this page and the others who have suffered from Depo deserve a voice! Does anyone know of any sites/groups that are actively working to change the way Depo is administered? I am scared for the young girls who are now making their first contraception decisions!
Thank you Laura, Lisa, Geraldine, and Dr. Prior for this page and for taking the time to listen and respond to the women here. I am thankful for the information and replies here!
I recommend probiotics for IBS. Favorite study supporting this is A Controlled 6-Month Intervention
by K. Kajander et al(Aliment Pharmacol Ther. 2005;22(5):387-394.) Showed steady improvement over the 6 months of the clinical trial on all measures of IBS with probiotics over placebo.
We know that oral contraceptives can disrupt gut flora (discussed briefly in “Coming off the Pill” by Lalonde and Matus), and many other dietary factors contribute to dysbiosis, as does antibiotic use. So intestinal illnesses are prevalent in many pops and play a role in various health matters from obesity to cholesterol, immunity, and so on. Point is – there’s often more than one factor at play in health and illness which is why we need to treat patients as individuals rather than a herd.
Have any of you experienced extreme anxiety/panic attacks while on depo and for months after stopping depo? I got my last shot in December 2012 and its now November 2013 and although I have gotten better the symptoms seem to keep changing…my bowel movements are rarely normal since the worst of the started in January. I was taken to the er twice in January and they couldn’t explain the heart palos other than I was “panicking” even tho I didn’t feel I was…until a week later when the intense anxiety hit me like a load of bricks…please feel free to email me I can use all the help I can get.
I will share any or all of my story to anyone who’s curious…
For a lack of period, Depo worked wonders. As a drug and long term treatment option, this was a nightmare for me.I was on it for 6 years. I’ve had the worst experience with trying to get my hormones back in balance since my last shot in April 2013. I had a 5 month long period and then had to fight the insurance company to cover an ablation because “Depo-detox” isn’t recognized as a reason for long term periods and they couldn’t call it medically necessary otherwise. Coming off depo, I experienced real suicidal ideation for the first time of my life. I am a trained social worker. Most horrible feelings ever that were related to the raging swings in hormones following the 14 weeks after my last shot. The thought that I was not prepared with any knowledge of the detox is horrifying for others. The drug company should be responsible for identifying the effects after long term use and its dangers of stopping. Doctors need to respect this as a difficult form of physical withdrawal, literally waiting game for hormones to balance on their own, and the info needs to be shared so that patients make an informed decision before they start taking it. And most certainly even if you’ve been on it and you want off of it, please doctors should not leave patients responsible for doing their own google searches to figure out the correlation between wanting to drive off a cliff and a female hormone imbalance. Drugs need to be studied to get on the market. Perhaps this one needs to be studied to get off the market.
I have been on depo shot for 19 yrs and have numerous side effects is this normal moody, night sweats and hot flashes its awful. I also have bad periods they are regular started right when went off depo also can I have children…Can you get tested to know if fertile?? When does these symptoms go away?? I dont like way I am feeling and its been 9 months off deposits so when does my hormones come back well I think they are now didn’t have these symptoms in beginning…please help thsnks
Hi Heather,
The answers to some of your questions can be found in the interview above under this question:
LW: Many women are told to just “wait it out.” This could mean months of not ovulating, ages without a menstrual period, or putting up with flooding menstruation. Do you think that’s a good idea? If not, what would you suggest?
Please go back and read Dr. Prior’s response to this question. There is a suggestion for treatment that may help you achieve regular fertile (ovulatory) cycles.
You don’t mention your age, but if you’ve been on Depo for 19 years, I’m thinking you may be in your mid-late 30s. You are experiencing some signs of perimenopause – night sweats and hot flashes. As noted above , Cyclic Progesterone Therapy, can help with this. If you go to this link you can download a handout about CPT to take to your doctor:
https://www.cemcor.ubc.ca/help_yourself/articles/cyclic_progesterone_therapy
All the best, Laura
I’ve been on depo about 12 years. I’m 49 and suffered from menstural migraines all my life. Pregnancy resulted in daily migraine during first trimester but disappeared altogether for the remainder of the pregnancies. Depo stopped my periods and the migraines. I’d sometimes get a migraine and crampy when due for my shot. Lately, I seem to get them on and off for a couple of weeks, though not quite as severe. Zomig helps but nothing else.
My doctor wants to stop depo when I am 50 (6 months). I am terrified the migraines will return. They are so painful and debilitating, I cannot bare the thought of their return. How likely is it these migraines will go away once I reach menopause?
Hi Patty,
If it is the higher estrogen that is causing your migraines to be so bad, then they will decrease and stop when you become menopausal (one year without flow).
I agree with your doctor that it is likely a good time to stop DepoProvera. However, you can’t do that comfortably given your migraine headaches.
If you have the time and interest to monitor your experiences, I’d suggest that you start keeping the Daily Perimenopause Diary https://www.cemcor.ubc.ca/files/uploads/Daily_Perimenopause_Diary_with_treatments.pdf now and record one whole DepoProvera cycle. Remember that in the headache line, if it is a migraine, put a dot in the box as well as a 1-4 for how intense a headache it is. Then you’ll know what is happening if you make the changes I’m suggesting.
Ask your physician for a prescription for oral micronized progesterone (Prometrium). When you are about a month before your next shot is due, start taking 300 mg (three round capsules) at bedtime daily. It may not totally take away your flow if you are still in perimenopause but it should help your sleep, any hot flushes/flashes or night sweats you might get on stopping Depo and will very likely prevent most migraines.
I hope this is helpful for you. If it is not, go onto the CeMCOR website and email for further suggestions.
All the best,
Jerilynn
I was on the depo for a year then me and my fiancé decided to try and have a child. I have been off for a year and a half and my periods r every 30 days but I still have not gotten pregnant. Do I have any on whay advice on what the signs r of getting my hormones back on track
Hi I seen this is dated back last year is there anyone I could talk to now I need help and advice… thank you!!
Jennie, Have you charted your cycles? Do you know if you are ovulating? How long have you had 30 day cycles for?
If you are interested in fertility awareness: https://holistichormonalhealth.com
My nurse recently, out of the blue, told me I should look for alternative contraception due to depo leading to osteoporosis in menopause if use continues beyond two years. I’ve been on depo since I was 21 as the pill gave me migraine. I’m 44 this year! I’m not sure where to turn or what course of action to take. The only information I’ve been offered is leaflets on the implant contraceptive. 2 years I’m 22 years over that.
I’ve recently been getting an odd hot flush and I’ve found my low moods (which I’ve always had) are perhaps a little harder to fight. I’m over weight but have had weight issues all life. I’ve no idea to stay on it come off it. If I should take a supplement or if I’m unique in the length of time I’ve been using it. I could become a study lol Any basic, straight forward information would be most gratefully received.
I saw this article while trying to look up answers behind my symptoms I’ve been having after quitting the depo shot and I can’t believe the amount of people who are experiencing these same things. I just turned 20 and I’m 115 pounds, I took the shot to combat my monthly almost paralyzing cramps. I took the shot for about a year, and quit in December when I couldn’t afford them anymore.
Since December, I haven’t had a period, I’ve been experiencing extremely sore breasts (I can’t even fathom wearing a bra right now, a shirt hurts bad enough), bloating and plenty of other digestive issues, anxiety and depression, heat flashes, and migraines to boot. At first I thought I had stomach ulcers but that is not the case.
My doctor never told me anything about the results of stopping the depo shot. and they were right when they said above that it affects young women who have never gained a lot of weight, and are under times of heavy stress. I just got laid off before my birthday last month and I’m moving away to college in August. it’s a stressful time.
I’m worried about my ability to have children in the near future and also how long will this affect me and the future me’s body?
email me erickawebb26@yahoo.com
If you decide to stay on depo, then you shd be screened for bone density so they have a baseline in your files and can monitor changes. Also consider supplementing with vitamin D and calcium.
If you decide to quit depo, then it will be a long haul to regain your healthy fertility cycles, but ultimately better for you because ovulation is beneficial for many reasons and suppressing it is not the best way to spend a whole adulthood.
I have been having major abdominal discomfort which has worsened over the past 5 years. I started taking the depo 5 years ago. I’m thinking this may be the problem. I am stopping my depo shots. Will let you know how it goes.
I have been on the depo for 17 years. I asked my doctor several years ago how long I could stay on it and he said I could stay on it forever. I loved not having my period and trusted him to know if the shot would cause problems.I must say I was very surprised to find out that it is only recommended for a couple years. I have been having chronic headaches and muscle pain for the last two years. I have been unable to find any long term relief. I am due for my shot in March which I will not be getting. I am terrified of what I may go through and if I will have withdrawal symptoms. I am currently looking for a new doctor and trying to educate myself. Do I need a bone scan? What can I do to make sure this goes smoothly? How can I find out if my chronic pain is from years of being on the depo?
try not to worry about the long use of depo until you see how it goes when you quit. You might feel better,or go thru a rough patch; either way, do record your observations as your fertility cycles return and note your headaches and pain levels. Tests like bone density and blood hormone levels may cost or depend on a doctors willingness to order them.
Collect your own data for free; what you eat, how you feel, how long between periods, signs of ovulation, temperatures, energy levels, many more factors. this info will increase your confidence when making decisions about your health. Self observation is the 1st step in any project. Next is to bring your food quality up a few notches and consult a practitioner as required.
I am 19 years old and was on depo for a year. My period stopped about 6 months ago and I stopped taking injections in January. I have gained weight, my boobs are sensitive and I’m really cranky and irritable. I’m wondering why I’m gaining so much weight since coming off of it. I lost weigh while I was taking the injections.
I am so relieved to have found this page. I was on the depo provera shot for 9 months, my last 3 month shot ran out on January 21st 2014. I initially was advised to go on the shot by my gynaecologist for extreme mittelschmerz, PMT, recurrent cystitis symptoms and heavy and long-lasting periods. To begin with it worked fine and then gradually the period type pains returned (but no period.)
My normal doctor recommended I come off the depo and use a mirena coil instead. I had that fitted at about week 7 of my last depo shot and then my shot ran out… Gradually I have noticed weird feelings of physical anxiety, minor hair loss, spotty skin, feeling ‘jittery’, feeling down, dizziness, joint aches and hot flushes.
The hair loss seems to have slowed down a but but the physical symptoms of anxiety are still present and are driving me mad!
I have previously been diagnosed with generalised anxiety disorder and depression but this was all completely under control and not a problem at all until I came off the depo provera injection! Plus, being well acquainted with anxiety thoughts and symptoms, i can DEFINITELY say that my ‘normal anxiety’ is different to this new, other ‘withdrawal’ anxiety…
I’m relieved to find I’m not going mad. But am I going to get better??
Someone please help. Email me directly if you like:
elizabeth_walker_harby@hotmail.co.uk
I’m 20 years old, I was on depo for 1 year I’ve been off it for a year 3 months now but I’ve been on my period for 5 months and it’s really starting to bother me. I don’t have insurance to go to the doctors so I haven’t seen anyone aBout this. I’ve been saying I’m going to call the health clinic but I’ve been putting it off because I keep thinking my normal periods are going to return. I wish I would have looked into different birth control before getting on the depo..
Im 17 years old I just got off the shot about 3 weeks ago. I had only gotten two shots. With the first one I was bleeding for 2 1/2 weeks each month for the first three months. Then when I got the second shot I bleed for 2 1/2 months! They gave me estrogen pills that didn’t seem to help much. I had god awful headaches, gained weight, horrible mood swings,my hair started falling out, and I felt like passing out all the time. Now that I have been off of it I have been bleeding for 3 weeks now and I have no energy im so tired all the time, my vision is blurry, I get headaches again, my acne has gotten awful, I feel like passing out again. What do I do? Im sick of this.
get your iron levels checked! you might be low from all that bleeding. Vegetarians shd supplement B12 and folic acid w iron supplements since they help it absorb.
sucha shame that so many young women are having their hormones messed with in sucha cavalier manner with no strategy for dealing with repercussions. Find a fertility awareness educator to teach you to chart your cycles and you’ll never need hormonal birth control again. I’m listed with colleagues at http://www.justisse.ca – Lisa Leger
I started Depo about a year ago after a miscarriage forced to by my mother to make sure i didnt get pregnant again. I was 17 and after my first shot my period stop completely. Nothing for 3 months. BLISS!! But once my time was up i began to bleed heavily but just for a few day, re-did my shot, not a drop of blood for another 3 months. Then we didnt re-inject my shot for about a month. Worst time of my life ever (at the time). I bleed the entire time it would not let up. I did not want to have the shot again since i wanted to get regular again. But my bleeding ended up making me BEG for the shot. Last December i knew my shot was wearing off and I am almost 18 now, but i thought if i get pregnant then i can handle it i’ll be 18 whatever. I’m done with that damn shot. Before i started it i was regular i knew the day and even the time i would start each month. Now? I have only stopped bleeding for about 2 weeks since December. That was almost 3 weeks ago. I am about to go on four months of nearly continuous heavy as can be bleeding. The color has changed from a dark color i was use to at the end of my periods to now a BRIGHT red as if i have a fresh wound color. I passed out when a nurse tried to take a small amount of blood for a test, and i give blood all the time, and i felt worse just getting a couple drops taken from me than when i give blood at a blood drive.
Now with my explanation done. Do i need to go to the doctor and get checked out? I will not go back on birth control, but i want this torment to end. Not just the bleeding but my sex life has come to a complete halt, not something either of us like. I don’t want to continue this blood lose, i have a blood drive coming up and i would like to give again but if this continues…Will i even be able to? Will there be an end to this torment that will still allow me to have children? I’m still three years away from the age we have decided we would start trying for kids, and i’m very excited about that. Will this affect my future child-baring years?
Also, i was just reading through some comments. The blood test i had taken that made me so sick and pass out was because i now am being tested for gallbladder problems. I can’t eat without getting sick.
And on the other hand by reading through the comments it is comforting knowing i’m not alone. I wasn’t told anything about the shot other than my mother had a bad reaction to it. My doctor injected me and told me i might gain some weight. I did gain a little but since quitting the shot i have lost 30 pounds.
How many times did you take the shot? For the person getting tested for gall bladder
I only had the shot 3 times.
I was on the depo shot for four years. I was concerned because I read that it can mess with your bone density as well as it can take up to two years to get pregnant after stopping. Instead of getting the shot I got a birth control pill instead. It has been three months on birth control pill and six months since my last shot. I was concerned because my periods have not returned and doctors did not warn me of any of this. I am 27 now and started the shot after my last child was born when I was23. I would like to have more kids some day but I’m very concerned and irritated that none of this was mentioned when looking at options. Thoughts or suggestions
Haley email me I only took one shot and the doctors were suggesting it was my gallbladder functioning slow I can give you more info on my experience erickawebb26@yahoo.com
I’ve been on depo for about 5 years. I started because my body couldn’t handle the pills and made me severely sick. I’ve finally decided to get off the shot do to extreme side effects it causes from prolonged use (no sex drive, inability to “get wet” {excuse my wording}, depression, anxiety, animia, ect.) I got my shot in January and now I have been bleeding for 3 weeks straight. I’ve talked to my mother who’s a obgyn and she tried giving me a new birth control pill to use hoping ill take to it and things will calm. However; it worked for a few days and then the bleeding happened again. This time darker and heavier. My breast became tender and I became to feel extremely tired, uncomfortable, and no appetite. I told my mother worried that the pills are not taking to me well (though its only been a few days) and she told me there’s a chance I could be pregnant. The test came back negative. I’m curious if I honestly could be or if something is honestly just wrong right now. The above article didn’t help much as I’m 18 and its talking as if these effects happen to older woman who are/would have been in menopause.
Get your mom the obgyn into an intellectual mood, then invite her to acknowledge that all hormonal birth control works by disrupting the endocrine system. This might be tough for a physician to admit. Your mom is uniquely challenged to restore the fertility of her own daughter. I say that she will not accomplish it by giving more synthetic hormones, but rather by practicing the fundamentals of good medicine and parenting both; which are simply that we assume the body works properly when there are few interventions, decent nutrition and not too much stress.
As a fertility educator with a 21 yr old daughter, I relate to your mother’s predicament and encourage her to think outside the box and apply her research abilities to the problem of helping you recover from the hormones.
I’m 19 and I was on Depo for about a year and didn’t have a period during that time (nor a sex drive for that matter) my period came back 6 months after my last injection (followed closely by that sex drive) and never stopped. It’s been 5 months now and I’m still bleeding, sometimes heavily, sometimes barely at all. It is the only problem I’ve had since stopping Depo but it’s becoming a huge burden (I am not in the financial position to keep myself in a regular supply of tampons/pads and have had to ask for help)
It also seems like though i bleed non stop I am getting ‘my period’, every month I will cramp just like i’m getting a period and the blood will even be bright at times. It really concerns me and to be frank i just want it to stop.
I’ve been on my period since last November 2013 I was on the depo shot for a year too but while I was on it i had my period twice while I was on it and they lasted for about 2 months each . my sex drive has not changed tho.. I’ve been off the shot a year and a couple of months now. I was 18 when I got on the depo shot. Have you went to the doctors Yet?
This is sort of an update to my comment a month ago.
I took some advice from this artitcle and the people commenting, took some ibuprofen to help with the non-stop bleeding. It worked amazingly, so thanks for that. BUT the surprising thing: the bleeding stopped. Two weeks after it stopped I had a normal 5 day long period. After nearly 5 months of what I before called torture, my life is now back to normal. It feels amazing and now with the ibuprofen trick, my last normal monthly wasn’t as horrible as I had once dreaded before my first shot. 😀 NEVER taking depo or birth control again. EVER.
Hi Haley, Thanks for checking in with an update. Glad to hear the info in this post was helpful to you. All the best!
Where is the article about the ibuprofen? I’ve been bleeding for 6months now and I want my periods normal again please. If you could send it to my email that would be great
Delfina.ceniceros@gmail.com
Hi, I’m glad I found this forum. I’m going through my own post-Depo hell now: breasts that feel giant and very sore, worse acne, nausea/bloating and hot flushes during the day. My sex drive however is amazing! I wondered if anyone had any luck with going back on something like Mirena IUD or Implanon rods? I wanted to be off Depo due to the bone loss issue (35 with no plans soon for children) and I thought my acne might clear up as well. I really need this bloaty, huge boob, pimply feeling to stop and I don’t think I can wait 6 months or more…
Hello Jessica,
Sorry you’ve been having horrible side effects; I had exactly the same plus terrible anxiety and panic attacks. I had the mirena coil fitted in the 8th week of my final depo injection. Unfortunately, after the depo gradually left my system it became apparent that my body didn’t agree the the mirena at all. I experienced hair loss, anxiety, nausea, crippling cramps and suicidal thoughts. I had it 3 months and then just had to get it out of me. A week after removal I was almost back to my normal self. However, I am still experiencing the awful breast pain and swelling and horrible acne, worse than it was when I was a teenager! Prior to the depo injection I was on the contraceptive implant which was actually good for the first year and then I started bleeding constantly; after 4 months of bleeding I had it removed. Anyway! That is just me and my experience, it could very easily be very different for you. If you want to chat please email me on elizabeth_walker_harby@hotmail.co.uk
Xxx
I had my last depo injection April 2013. I didn’t have periods while I was on it and finally showed signs of what seemed like a period around March 10, 2014. It was light and only lasted about 4 days. But since then, I’ve been bleeding every two weeks. I know it’s normal to have abnormal bleeding after stopping depo. But, how long will I take for my periods to be normal again? Has anyone else experienced this?
Hi im 17 years old i started taking depo last year july 2013 then had my next shot at october. My 3rd shot was supose to be at december 29 but i decided to stop due to painful headaches. I had mood swings and feeling so tired. This may 2014 i dont know if this was ,y period coming back after several months one day i experienced having brown discharge then the other day. I have red discharge then it came out as a brown discharge again i’m so worried i’ve taken a pregnancy test and it cAme out negative. Is this an effect of stopping depo and starting to have my menstrual period back?
To 17 year old Fatima – please dont worry sweetheart. There is lots you can do to have healthy fertility cycles. Sometimes brown discharge can be a sign of trouble that needs to be looked at, but usually its just some oxidized blood coming out. Its normal to have weirdness when quitting depo, but your cycles will likely return on their own in time if you avoid hormonal drugs. Meanwhile, eat healthy, learn how your fertility cycles work and stick with condoms. We’re all supposed to be using condoms all the time anyway to protect us from diseases and they protect us from pregnancy quite well, too.
Hi Natalie – lots of women have experienced what you have. Rest assured that your cycles will likely come back to normal on their own. At least now you know you’re probably not a good candidate for hormonal drugs. My best advice is to eat healthy, stay fit, learn how your fertility cycles work, and use condoms all the time.
Lisa,
It has been one year since I first posted about my “positive” experience receiving my first AND LAST depo shot. I’ve been following these comments religiously and they have been very helpful. Thank you.
Here’s how it went for me: Depo Provera was the WORST thing I ever did to my body. I ended up getting a Paragard (copper IUD with no hormones) in July of 2013 instead of another shot and that was probably the BEST thing (or will be long term). However, in the meantime I experienced:
1. unexpected weight loss – I quickly went from a healthy 140 down to 126 last summer and can’t gain anything back. I look emaciated.
2. no period at all from August 2013-March 2014. blood test showed I had no menstrual hormones at all. The doctor thought it was because of my weight loss, but from these posts I’m convinced it was the Depo (which also probably caused the weight loss!!!)
3) the past 2 months I’ve been bleeding every two weeks very heavily for about 4-5 days. My only savior is a menstrual cup, which I recommend to any lady because you don’t have to worry as much as a tampon and it doesn’t leak (gotta be careful with IUD strings though).
From your comments I’m confident my cycle will normalize in time now that I’m off hormones for good, but it’s a frustrating road to get there!! Thank you Lisa for all your support!!!
Thankyou soo much. Im so glad i fount this site 🙂
How long does the withdrawal last
I am 35 years old and got my last shot in late January 2014. I have been on it for 15 years. Tried the patch and ring at one point but loved the simplicity and freedom from the shot. Now my husband and I want to start a family. My breasts feel incredibly tender, achy and huge. Even wearing a bra most days hurts. The fatigue is crazy and came on like 2 weeks ago. Sex drive is still great. Weight gain and bloated feeling are driving me up the wall. Waiting to see when my period comes back and how long until we get pregnant. Doctors say up to 2 years. No one ever told me to change my birth control. In fact she said if it works, just stick with it.
Hi I am now turning 20yrs old went on Depro after I had an abortion @ 17 yrs something I’m really not proud of syill haunts me…anyway I’m due for my next shot this month which is May & have decided not to go cause I don’t want to take it anymore, I’m really confused though because a few weeks back I had a bladder infection & had to go on some really strong antibiotics & it was 2 different ones because when the other one did not work they referred me to a different anti-biotic is it maybe possible that now the depro might be out of my system & that it is likely for me to fall pregnant?
When stopping Depo or other hormonal contraceptives it is helpful for a woman to seek counsel from someone trained in these matters. Justisse Holistic Reproductive Health Pracitioners (HRHP) teach women how to prevent pregnancy by using fertility awareness methods and are specifically trained to help women wanting to stop or recover from hormonal contraceptives. HRHPs as well as some complementary or functional medicine physicians, naturopaths, nurse practioners or midwives are knowledgable about how to help women recover their sexual and reproductive health.
I’ve been on Depo for a year and a month. I’m due for my shot on June, but I wont be taking it, as I have been experiencing a lot of joint pains, headaches, sore breasts. Has anyone else had the joint pain issues?
I’ve been on Depo for a year and a month. I’m due for my shot on June, but I wont be taking it, as I have been experiencing a lot of joint pains, headaches, sore breasts. Has anyone else had the joint pain issues? It has me worried that it can be something else?
I am 34, have one 6 year old, am a healthy weight, and was on the depo for 9 months. No period the whole time I was on it which was great, but every time I was due for my shot I would have headaches,nausea and depression. When I would get the next shot, I had horrible mood swings to the point it almost ruined my relationship and severe acne outbreaks. I did not want anymore children so I had the Essure procedure. it has been 6 months since my last depo shot, and only my third period first two were very light and spotty but the third was normal for three days, and then seemed to stop but started back up the next week very bright red which is unusual for me and hasnt stopped. Two weeks now so was concerned. I am going to try the ibuprofen to see if works, happy to hear it worked for someone else. Will Check back in if it does 🙂
Also very sore breasts, headaches and insomnia, nausea. I read and signed the symptom form provided by my doctor but it and most medical studies state return to normal after 6 months….reading all the posts from all the women concerns me. I think depo is fine for offering to woman, but it looks like the side effects and types of woman taking it should be looked at more closely and updated on the warning sheet you sign before considering.
I would not recommend the depo to anyone unless a last resort.
I’m 16 years old, and I had been on Depo since November 18,2013. While I was on it, I experienced mood swings, headaches, abnormal pains, bloating and fatigue. After a week of me first being on the shot, I had gotten my period but it has been continuous bleeding, and never went off! It has been like a regular period, it would be heavy then become light but never went off. I only took 2 shots of the Birth control because I did not want to go through another 3 months of continuous bleeding. My last date to take my shot was april 29th, however I didn’t go, but I am still having continuous bleeding even though I have stopped taking the shots. I’m depressed and wondering when will I ever stop bleeding. I wouldn’t recommend this method of birth control to anyone !!
I am 21 years old nd i had my first shot in january 2014. On march i ws suppose to get my second shot but i decided to stop. I have not got my periods since then and its worrying me.
Hi, I had taken my only depo shot on 27th Aug 13, had spotting after 1 month , never went for the 2nd short due to the side effects , had put on 5-6 kgs which is not decreasing , I am 34.Untill now my regular periods have not returned… I am bleeding from last 22 days… this has become a regular practice from December.Please suggest a remedy
I got first depo in November 2013 and was supposed to go back in February 2014 but didnt because It made me really bitchy and didn’t want hubby around me and my two kids where driving me crazy. I started my first period in May 2014 I wanted to know if I can get pregnant??
Ive been on depo for about a yr.. My spotting never stopped for over a year but 3 months adter my last shot my spotting stopped and 1wk after that,my menstruation came back and stopped after 7days and after that,it never came back again..its been 2monts now.. Is it true that the depo will last 9-10m after your last shot? Is spotting for months the reason why i dont have periods now? I look pale, my lips are pale..lol
I had been regular with my period before I had my first depo shot. I took it for the convenience that my first time with my husband would be natural. I had it May. For the past week and half, I have been getting vagina bleeding. Anybody know when if will stop?
I was hoping that I would not have to brings pads on my honeymoon. Please help.
I had been regular with my period before I had my first depo shot. I took it for the convenience that my first time with my husband would be natural. I had it May. For the past week and half, I have been getting vagina bleeding. Anybody know when ii will stop?
I was hoping that I would not have to brings pads on my honeymoon. Please help.
Depo is so boring with many side effect,heavy weight at back,depression,loss hair,feeling to kill yourself,there so many including bleeding,there worst part is Doctors they don’t know how to help.gall stone when u leave it.
Hmmm, I’ve been on Depo (or devils drug) for 20 years – yes I missed the tdon’t stay on it for long memo as well. Mine is for endometriosis that I’ve had 5 ops for and up to 40 cyst layered each time.
I have mine every 11 weeks as the depression, pain , anxiety and paranoia at 11 weeks is to difficult at work. I’ve suffered 3 lots of pneumonia, a flu every year, irritable bowl, night leg cramps, several fractures, my bones are a jagered mess, I’ve osteo in hips and knees and waiting to see an Endo for a RA diagnosis I also have random full blown anaphylaxis to random drugs and foods!
I’ve been told I’m to switch to marina implant and have decided to come off Depo – it’s week 13 since my last injection and wow I’ve not missed the pelvic pain of Endo!
I’ve been prepping for a year, lost 18kg, only eat whole foods and now take Spirulina and brewers yeast, I’m hoping this gets me through the other side affects!
Needless to say I am very scared!
I was on the pill for about 3 years before I switched to the shot. After my first shot I bleed every day for those 3 months, but the doctor said it needed more time for my body to adjust. 2 shots later, I still bleed every day. I switched back to ortho tri cyclen which has the sugar pills first and my bleeding stopped. Should I be worried my period didn’t come during the (first) week it should have? I just find it strange my body bleed for so long and stopped at a weird time. I don’t have morning sickness or sore breasts, just some cramping.
We can assume that the hormones caused the abnormal bleeding and being off them for that placebo week allowed your levels to normalize and the bleeding to stop.
We used to call that “break through bleeding” in the earlier days of the pill and doctors wld usually switch women to a different type or dose when it happened. This sometimes worked out OK, but as Holly says in Sweetening The Pill, there are likely far more women out there with side effects from these powerful hormonal drugs than we realize; partly because of menstrual taboos that make us suffer privately and partly because medical system minimizes the problems and fail to report them.
May I just comment that the women posting here about their depo experiences remind me of the canaries that miners used to take into coal mines to monitor the air quality. If things became too toxic, the canaries wld sicken or die thus warning the men to get out before they were harmed. Those women w side effects inform the rest of us to stay away.
Now we have Vicki with irritable bowel, osteoporosis, anaphylactic allergies and a possible auto-immune disease. Her doctors must take a more wholistic approach where the whole history would be taken including past hormone use. The Rheumatologist sld not be allowed to look only at her inflamed joints and her misbehaving immune system and treat them as isolated from her IBS and allergies. Its so frustrating, because its all connected. Now this case is so complex that it will be a big challenge to fix everything. To help Vicki deal w the IBS and allergies, I wld emphasize probiotics. The good bacteria are your new best friends VIcki, take them daily to correct the environment in your intestines which will help proper immune function and reduce food reactions and inflammation. I recommend finding a Naturopathic Physician who specializes in women’s health. You’ll be giving them quite a challenge, but your weight loss indicates that you are disciplined and motivated to make the changes that wld be required to get better.
Hey there. I’m 20 years old and have been on the shot since January of 2010 I believe. I’m ready to go back to having a normal period and I plan on going to the doctor next week to see my other options as far as starting another form of birth control but I’m curious to know if I should wait till I start getting my periods regularly again?
Also I was wondering if being the Depo shot for to long can cause your body to become infertile entirely? I know with out a period you can not get pregnant but what about after I get my period again? Do I become fertile again or is there a chance that I might not be able to have my own children one day? I’m kind of freaking out!
And if any one has changed from the shot to another form of birth control in a short amount of time, which one did you change to and how was it after?
My last shot was January 23rd 2014. So I’m just at 4 years give or take by a week or so. Any response would be great.
check out natural birth control methods that use fertility awareness and barriers. Hormonal drugs are endocrine disrupters, they work by disrupting your endocrine system. [not cool]. If you learn to chart using the Justisse charting app at http://www.justisse.charting.app.com or something similar, then you will not only know exactly when you’re fertile times are, but you will also be able to use your charts as a health record and diagnostic tool to monitor the return of your fertility. Also – you will likely ovulate before you get a period [what usually happens] so its “conceivable” that a girl cld get pregnant before she even gets a period. So watch it, we’re all supposed to be using condoms all the time anyway, right??
Well Ive always had a hard time using latex condoms. So my boyfriend and I are going to try other kinds. But thanks for the chart idea! I’ll have to check it out!
One last thing, it’s been over a month since my last shot was due, should I be expecting a period soon?
I just found this site.I am a 50 year old woman. I stopped depo 7 years ago after being on it for 15 years straight. while I was on depo I had no periods. and I had no other symptoms. Or so I thought. Towards the end of my depo use, I had gained 100 pounds, I was depressed and had panic attacks and I had acne. My bones started to hurt and my joints are started to ache. and no one connected any of it to my depo use. Since I stopped the depo I’ve been diagnosed with rheumatoid arthritis, lyme arthritis, and a wide variety of other arthritis. I’ve been diagnosed with geriatric osteoarthritis and I have suffered 5 bone breaks in 2 years. I recently broke a thumb when I tapped it on a desk. and it won’t heal and it’s been a year. Within the last two weeks I was diagnosed with a broken hip and I have done nothing that would break the hip. there’s a possibility that the other hip is also broke. And now I’m looking for a doctor to look into the possibility of hip necrosis. I cannot work I cannot ride my horse I can barely function to the bone pain that I deal with everyday. and the doctors have no idea why this is happening but they aren’t listening when I try to make the connection to make the connection long term depo use. This blog is the first right of hope I have had. Thank you so much for being there
Glad I found this article. I was on Depo for two shots, had normal (but kind of heavy) bleeding during first shot cycle, during second, had nothing. My sex drive completely disappeared while being on it, and after being off the shot for 5 months (since last scheduled shot), my normal menstrual cycle has not returned, no bleeding, and no obvious ovulation (used to have mittelschmerz). I felt horrible for the first few weeks after I did not go for my next scheduled shot, and figured, at 38, with no romantic partner, I was really just doing it to avoid the mittelschmerz issues and aggravation of heavy and painful periods. It may sound stupid, but I want my periods back!!! I am afraid I have catapulted myself into some state of early menopause, my hormones just seem to be at a standstill. I had a little weight gain while on it, not much, and my breasts were sore during the shot, and still now, but it is manageable. My biggest concern is that I have just screwed my hormones up to the point my body thinks I’m done with everything. My mom went into menopause late, and bore children late in life, as have most of the women in my family, and I have a grown daughter, had her when I was a late teen. I hoped to maybe at least have one more kid someday, but I’m scared I won’t even have the option to have another child, if the right guy came along, and we wanted to. It’s sad. So sorry to read other ladies’ stories.
I have been on depo for 2 years, my last shot was in January and I didn’t go back for my retake in April, am I at risk of getting pregnant, how long does it take usually to be able to get pregnant ? I don’t want to be pregnant and I’m kinda freaking out because I’ve had unsafe sex, PLEASE HELP ME OUT HERE ASAP
I have been on depo for 2 years, my last shot was in January and I didn’t go back for my retake in April, am I at risk of getting pregnant, how long does it take usually to be able to get pregnant ? I don’t want to be pregnant and I’m kinda freaking out because I’ve had unsafe sex, PLEASE HELP ME OUT HERE ASAP, I need to know soon
I have been on depo for 6 months my last shot was from last week Wednesday bt I didn’t go for it. I had sex this week is there any chance that a may be pregnant?
To those fearful of pregnancy after quitting hormonal birth control. 1st, let me just remind you that we are all supposed to be using condoms all the time to prevent disease and condoms also happen to be effective for birth control. If you need a refresher on this, just drop in to your local public health nurse and she’ll set you straight on the subject of diseases and condom use. 2nd, knowing where we are in our cycles is useful and easy once you know what to look for. It’s like knowing when you’re hungry or have to poop; you just pay attention to your body signals, right? I recommend learning a fertility awareness method via one of the many online teachers or apps. Better still find a local teacher in your area for personal instruction. This involves observing cervical mucus when you wipe after using the toilet (it means you’re fertile), and keeping track of what you see. This practice helps you avoid pregnancy by alerting you to fertile times in your cycle and also gives you a useful health record as your fertility cycles return to normal. The whole point of charting your cycles is so that you dont live in fear of pregnancy but in joy and acceptance of your healthy cycling body. I have taught the Justisse method for 25 years and have seen women move from fear and confusion about their fertility to confident in their ability to identify the fertile and infertile times in their cycles. Its easy and fun when you apply a bit of attention to the process. http://www.justisse.ca or http://www.justisse-charting-app.com for details. So – if you dont want to disrupt your endocrine system with hormonal drugs, then getting to know your fertility cycles is useful whether you use condoms or not by giving you more info about your fertile times. This also reassures you that your cycles are healthy in case you do decide to become a parent in the future.
Lisa, thank you so very much for your ongoing comments in support of the readers of this blog post who are looking for information about their cycles, fertility and pregnancy risk after quitting Depo-Provera.
I think the crystal-clear, take-away message for anyone who is considering stopping or has stopped using any form of hormonal contraception – be it Depo, pill, ring or implant – is that you must be willing and able to use condoms as a back-up method until you decide what to do next. If returning to healthy, ovulatory menstrual cycles is your goal, then as Lisa suggests here, using condoms while learning the fertility awareness method, preferably from an instructor, is a recommended course of action.
Just coming by to post an update. I know many women want to know whether those suffering from depo withdrawal come out the other side. It took 10 months for my cycle to return to normal, after stopping the shot (14 months after my last shot). I was on depo for over ten years.. had *horrible* symptoms from getting off it. I bled for three months straight and then it went to something weird like week on, few days off, week on, few days off, etc. Then every two weeks and finally monthly. I had a wide range of symptoms and every last one has resolved itself. So hang in there. It really does get better (and believe me, I didn’t think it was going to.)
I echo Laura’s thanks to Lisa Leger for her on-going supportive advice to those worried about their Depo Provera use on this list.
I also wanted to respond specifically to a post by “L” last week who said, “It may sound stupid, but I want my periods back!!! ” It doesn’t sound stupid at all. It sounds smart! Periods are not only a sign that your body is in working order; they are a requirement for fertility. I will always remember one the women from DAWN (DisAbled Women’s Network), who presented at Canada-wide hearings about Depo many years ago, commenting that she did not like having “the shot” because it meant losing her periods which was something that made her feel “normal”.
Im 18 years ol I had my first shot in December 2013.. for about 3 weeks I was having dark brownish clots and drainage but I never bled. It is now june 2014 and I hace yet to have a period or anything. I want to get on the pills so I can have my period again but I dont know if it is safe? I was told it takes 6 Months for it to get out of ur system.. so what can I do or whst do I do? With me not having the cycle I am bloated and really moody.. please help.
Ive only been on depo for a 3 months. Its time for my second shot (from the 3rd of June to 17th)… however ive been experiencing brown discharge for some weeks now. And lately is been getting worse. For a day I experienced bleeding and i wouldnt say a day more like 10mins in the am i used the bathroom and there was blood like a menstrual on my tissue. Then it went back to spotting brown discharge. Should I be worried? After the first injection my cycle stopped completely besides those 10 mins of that morning. My first injection was in March. In the middle of may the brown discbarge started closer to the end of may the incident with the tissue… now is time for the second shot and tbs discharge is increasing. Is it bc the second shot is due?..
I only had one shot in feb 2014. I was due for my second shot 2 weeks ago. I was doing fine and then out of the blue I started getting severe pms symptoms 4 days ago and started bleeding today. But I just had my period last week?!?! So what’s up with that? yesterday I started getting severe stomach cramping, diarrhea, headaches and nausea. It has not let up. Can one shot really mess with you that much? I feel like a mess 🙁 and no I am not sick with the cold/flu.
Thanks
There is a big body of medical literature about increased risk of osteoporosis with depo provera. Your doctors wont have to look very far to find it; its in their very own professional journals along with any osteoporosis agency like Osteoporosis Canada, the US version, and the international agencies. Their very own guidelines talk about the connection. It is very common knowledge among anyone who works in women’s health issues. I would be surprised if a doctor was not informed about this.
sorry Shay – being on the pills to get your period is not a solution since that fake bleed you get between pill packs is not a real period. Is a withdrawl bleed built into the system so women will feel “normal” while on the pill. If you want to have actual menstrual Periods, then stay off hormonal drugs and let your cycles unfold on their own.
yes, hormonal drugs can mess you up. In fact their mechanism of action as birth control is to mess you up on purpose for that you will be infertile. Thats how they work. If you want to have normal healthy cycles, then avoid hormonal drugs altogether and use natural means to avoid pregnancy like fertility awareness and condoms for example.
What about Depo Provera and the thinning of the uteral lining? Have more studies been released on this effect?
Been on depo for 2 years straight because of endometriosis pain. I’m 39 years old now and I must say that my experience with depo was pleasant. no bleeding which meant a break from the excruciating pains, I had absolutely no problem with my sex drive as a matter of fact I think that it increased. anyway I decided to get off depo with hopes of getting pregnant, however the withdrawal symptoms has been terrible. I’m incredibly moody and has severe anxiety, even suicidal ….. sorry but I think abb dying very often; however my partner has been very supportive. got my periid back and was kinda happy as it was not painful. However the second cycle after the shot was quite the opposite. …. I’ve bled for 8 days straight at first brown and ugly then unto rich red. I read somewhere about perimenopause and I’m terribly scared about going into menopause before I can have my first ever pregnancy.
Treating someone w depo for endo is medically justifiable, but its a far too invasive endocrine disrupter to be used as any other option on the birth control menu. Whatever reasons these women have for quitting, we hear similar difficulties with return to healthy fertility. When yours werent healthy pre-depo, then all the bigger challenge. I recommend a big health kick; do all you can manage and afford, see a Naturopath, try changing ur diet, supplements. These measures can reduce period probs, treat endo, and help w recovery from hormonal drugs. I noticed an old power point of mine that wound up posted online, its at: https://www.slideshare.net/seanenns/owtv-fibroids-and-endo
So I’ve been getting the shot for about a year and a half now after I had a c section with my son and I am now experiencing heavy bleeding for a couple days now but also now having clumps of the blood coming out with the bleeding so that’s what’s worrying me the most I’ve had spotting randomly throughout my time on the shot but usually nothing and I’ve had the cramps with no period and they weren’t normal cramps it was more like stabbing feeling …I’m juts more. Concerned about the clumps of blood and I would love to do ssomething about the bleeding so it’ll slow down or just end soon but I’ve had issues taking ibprophen so I want to know if there is anything else to take
Of course these probs are hormone related and getting off synthetic hormones is my 1st choice to solve them.
However, I suppose a person could try taking bioflavanoids. I recommend bioflavanoids for prolonged menstrual bleeding because they improve the integrity of small veins and capillaries (makes ’em less leaky, so we use it for spider veins, varicose veins, etc). Ask your health food store staff for a “citrus bioflavanoid combo” it shd have around 300-500mg per capsule and women often need to take 2 per meal with some Vit C to get results, but when it works, it dries up the bleeding within 1-3 days. Note – this is acting on the capillaries that feed blood into the endometrial tissue, its not doing anything to the hormone picture and thats where the real problem lies. Please consider quitting hormones, they work by disrupting the endocrine system, not good.
I’m so scared when I started the shot I got bad cramps for a few weeks but it wasn’t heavy then I got off the shot and experiance breast pain please help
I was on the depo shot for 3.5 years. It took a year to get my period back and 18 months to get pregnant. After my son was born I have been on and off it for the last 9 years. I have never had any of the other problems other women have. It just takes a while to get my cycle back. But I’m not complaining about that. I LOVE not bleeding every month. It’s the only birth control I can take because of very bad migraines. My cycle has always returned. How long it takes depends on how long I was on the shot. I know it effects everyone differently, and people are more likely to post a bad experience than a good one. I just washed to post my good experience so that people know that it does work for some people.
The bigger issue is the long term effects of depo. Canada had banned the drug due to the bone density issues of long term use. Many women have faced major joint issues such as arthritis, osteoarthritis, osteoporosis. Using the drug long term drops estrogen levels which leads to these and other issues. Whether or not it’s nice to have a period or not have a period, or how long it takes you to get your period back, is not the primary medical issue. We have to look at the long term effect of this drug on our bodies and make smart decisions. not decisions based on how convenient it is for us to have periods are not have periods! this drug is a bad drug due to the long term side effects not the day today conveniences are inconveniences.
I never once said I made the decision to use Depo because it’s a convince to not have a period. All I said was that it was a bonus. And I made the comment about how long it took me to get my periods back because based on the comments I read on this article that seemed like a huge concern to a lot of women. I take Depo because it works for me. I have been on it for about 10 out of the last 14 years. I have had two bone scans done because of the fear of bone loss.. They were both completely normal. I need the drop in estrogen. If I’m not on depo I have 2 to 3 migraines a month that take me out for 2 to 4 days. When I’m on depo I have a migraine once every 3 to 4 months. The two times I tried to take the pill I didn’t last two weeks without having horrific migraines. So for me it’s worth it. It’s not a bad drug for me. I have had several conversations with my Dr. about depo versus IUDs. The only stories I have heard about IUDs are bad stories, but I guess the same could be said for Deop. That’s part of the reason why I wanted to post my good story. I know not everyone will agree with me and that’s fine. Like I said I just wanted to get my positive experience with Deop out there.
If this article is accurate why is my doctor prescribing me the birth control pill (as he explained primarily estrogen) to combat this issue? He said I needed estrogen, not progesterone, the exact opposite. I am scared to take it because of how horrible coming off depo has been. I have had all of these issues coming off depo and more. I finally found a doctor that explained what the issue was at least (surprisingly the doctor that prescribed me depo told me there was no way my symptoms were caused by stopping it), but I don’t want to make things worse by taking even more estrogen.
Valerie, Point of fact, Canada has not banned Depo Provera. It is still prescribed, though much less often than a decade ago.
Thank you for sharing your positive experience with Depo-Provera. You are right that women are more likely to share negative experiences than positive ones, but as the author of this post it is disconcerting to keep reading week after week-on this post and the previous one I wrote about coming off Depo- how many women do have problems using and quitting this contraceptive. It is also frustrating to see how little doctors and sexual health care providers understand as to why and what women so often experience when they stop taking Depo. All the best.
Danielle, your comment illustrates how little most doctors understand about the endocrinology of the menstrual cycle and the effects of unopposed estrogen, which is what you are experiencing. Dr. Prior, an endocrinologist, has studied ovulation and the menstrual cycle for over 40 years. You decide who knows more about what women are experiencing when they stop Depo and why.
You may want to consider your age, your future plans for having children, your birth control requirements, and your health priorities before making a decision about how to proceed. One thing is certain, taking the pill is not about recovery from Depo, but rather the exchange of one synthetic hormonal profile for another. All the best.
Please read timeline re: when depo passed & where
https://www.bigclassaction.com/lawsuit/depo_provera_contraceptive_osteoporosis_class_action.php
most women’s health organizations called for depo to not be approved @ that time & most still call for its ban.
The bone loss issues lead to 700 million dollar lawsuits in canada. Problems with bone density, osteoporosis were the reason for “black box
warning” on long term usage. Current lawsuits in US around bone density issues are being filed currently.
Thank you Laura for your response. My question is what I should be doing about the symptoms I’m having. My doctor is concerned about severe anemia at this point because of the amount of blood I’m losing ( I’ve been bleeding heavily for 2.5 months) and that is, according to him, why he recommended birth control. He said there are other options if I’m not comfortable with that but I don’t know what I’m supposed to request. My health priority is I want to get better. My husband and I want to have children now. I’m 29 years old and I’ve been life disruptingly sick for over 8 months now, and stopped taking the shot 10 months ago, while we want to have children we couldn’t even consider it until I’m better because I’d be unable to care for a child right now, I can barely get through my day. I have no birth control requirements – I want to get pregnant and I use NFP anyways. I am looking for how to get past this, because I can’t imagine another 2 years like this as I’ve read some people have had. As I’ve been bleeding it’s gotten progressively heavier and I get cramps now every other day and they have gotten to be extremely painful.
The doctor showed me that I have a cyst in my ovary (he said that could actually be good news, he said the edges are starting to collapse and it could be a sign of returning ovulation), and that the ultrasound can’t even pick up a depth to the width of my uterine lining, which is why he thinks I’m bleeding so much now – he said I’m basically down to the muscle wall and that is constantly seeping blood, he said that estrogen builds up the uterine wall and that is why he wants me to take it (in the form of bc, but he said I could do the natural form if I was more comfortable with that).
So while I’d like to be flippant about this doctor being wrong, I don’t live in a place where there is an endless supply of doctors, and I’ve already been to five over the past 6 months and he is the first one that at least gave me an accurate read on the cause. He also said he wanted me to use bc because he didn’t suggest getting pregnant before the depo is out of my system as that can cause problems with fetus development. He explained that the depo shot is oil based and that’s why it hangs out for so long in your system.
Anyways, unless you know a doctor in Western Montana that can help me, I’d imagine that this doctor is my best bet in that he is the first one to not tell me that this is some weird form of depression, or anxiety, and to take my symptoms seriously, be able to explain why I feel this way and what is happening to my body, show compassion for it and try to help. I have constant daily bleeding, every other day cramps bad enough that Advil/Midol taken at twice the recommended level just gets me to a point that I can walk around, severe exhaustion but poor sleep (I have a device that measures my sleep and I get very little deep sleep a night and it is constantly interrupted by light sleep), severe memory fog (I will ask my husband a question and then ask him again a few seconds later – when this first started we would get in fights when I’d ask a bunch about a sensitive topic because he thought I was just trying to be a jerk,) hair that thinned so quickly my hairdresser thought I started dying my hair or something, dermatographia, constipation that continues regardless of diet, excercise, water, and medication, and severe weight gain (I was 135 pounds 8 months ago, now I’m 163, even when I sprained my ankle and couldn’t exercise for months the most I’ve ever weighed was 150 pounds, and I have an active lifestyle that hasn’t changed and eat primarily food I cook myself from whole ingredients, no junk, though the cravings for sugar I’ve been getting with the constant period are tough).
So I’m asking for what I should be doing and asking him in order to recover from this, what options there are for making the bleeding stop and helping me get my life back, because I’m at a point where it’s day to day, actually hour to hour, whether I’ll even be able to function. I am scared to take anything, and I’m scared to keep going like this. I just want to be healthy and able to start a family with my husband. Thank you for your help.
Hi Danielle, I’m sorry for the extreme adverse effects you are experiencing. Your age and future plans to have children do make a difference in deciding how to proceed. I’ve asked Dr. Prior to respond to your inquiry with the additional information you have provided.
If you haven’t already, I recommend you click through to the articles on managing heavy flow: https://www.cemcor.ubc.ca/help_yourself/articles/managing_menorrhagia
and the use of Cyclic Progesterone Therapy:
https://www.cemcor.ubc.ca/help_yourself/articles/cyclic_progesterone_therapy
Your body is trying to get back to normal cyclic function. Beyond the treatment ideas found in this post, you may want to consult with a Holistic Reproductive Health Practitioner on nutritional and other ways to help you restore menstrual cycle health. Lisa Leger is an HRHP who has responded to many other comments on this post. You may want to look through the comments for her suggestions.
Hope this is helpful. Hang in there. It will get better.
This is a response to Danielle who has been having heavy flow for 2.5 months, cramps, weight gain and difficulty sleeping after stopping Depo-Provera 10 months ago.
See if I can explain–when you were on the Depo, it suppressed your own estrogen levels. When you stopped it, your body was trying hard to get back to normal. It is easy for a woman to make estrogen, but it takes excellent coordination of many systems before it is possible to ovulate and thus make progesterone.
If you want to try combined hormonal contraceptives for a cycle to work with the new doctor that you trust, I certainly can understand. However, I wouldn’t give it more than one month’s try.
In the meanwhile:
1) on every heavy flow day, take a 200 mg ibuprofen tablet with each meal. That will decrease the amount of bleeding by half; for cramps, take 2 pills initially and take a further one as soon as the cramps start to come back.
2) Keep the Menstrual Cycle Diary https://www.cemcor.ubc.ca/files/uploads/Menstrual_Cycle_Diary_with_treatments.pdf so you’ll know for yourself what’s going on. If your breasts are at all sore, it mean you have a high estrogen level. If you have stretchy cervical mucus it means not only high estrogen but low progesterone levels. Here’s a link to the first of four YouTube videos describing how to complete the Diary and what your experiences mean: https://www.cemcor.ubc.ca/help_yourself/handouts/daily_diaries.
3) Since you were told you have anemia, and are bleeding a lot, it is most likely because you don’t have enough iron to match what you’ve lost with flow. I would take one ferrous gluconate tablet a day (these are over the counter in Canada although you have to ask the pharmacist) for one whole year (to build up depleted bone marrow iron stores.
4) You could start cyclic progesterone therapy any time you are ready (and have a prescription for it). Take 300 mg at bedtime every day for at least one full month. Then follow the instructions in the link to Cyclic Progesterone therapy that Laura gave you.
Most important of all–believe that your body has the power to restore balance (with a little help) and that when you are ready, you’ll be able to ovulate, get pregnant and carry a healthy baby. Keep up your good habits so that day will come sooner.
All the best,
Jerilynn http://www.cemcor.ubc.ca
I got off the shot about two months ago and just started my period for the first time yesterday. My question is, is it going to be normal now, about a week of bleeding every month? Or will I bleed for a long time? I see everyone has different side affects just wondering if this is something that is different for everyone as well or if i should expect blood for a while?
Brianna, from my experience on and off the depo shot over the years it just depends. I would say if you start having normal week pong periods two months out you’re very lucky. It usually takes a year for me to start having normal periods. I’ve never bled for more than 10 days but I know other women have. I have also had shorter periods that last only 3-4 days. It really just depends on how long it takes your body to get the hormone levels back to normal. It really is different for everyone. We can all tell you our experiences but yours could be completely different. I hope this helps you.
I spoke to my doctor and explained to him, my concerns on depo as I had it before (1 shot) and immediately got off of it as I bled for 6 months straight and I had a serious loss of libido. This time around he said, he would prescribe me estrogen pills, to help with the irregular bleeding. Is this common? I also, wanted to know what I could do if I do lose my libido again, I heard Maca root pills would possibly help, anything else you would suggest?
hi there,
i stopped taking the depo, my last shot was oct i think.Do you have to wait any certain time to go back on the shot after being off of it?
thanks much!
I am pleased to report that slowly, my body seems to be getting back to normal… Even though my ‘normal’ consists of heavy, painful periods, intense PMS, painful ovulation etc etc, it is preferable to the sever anxiety and depression caused by depo and then perpetuated by the mirena coil…
Currently for birth control my long term partner and I are relying on latex free condoms (I’m allergic to latex). My doctor has recommended I avoid all hormonal contraceptive methods in the future if at all possible. I would like to know, therefore, if anyone had any experiences of being on the copper coil? It is really the only option left to me… Any shared experiences much appreciated!
ughh – a Dr using a drug to treat the side effects of the 1st drug…. How about Not taking any synthetic hormones at all? how about Not disrupting your endocrine system? how about letting your cycles unfold naturally? I know, it sounds radical, even revolutionary, but its actually sensible and adaptive to avoid things that make you sick.
hi,
i have been wired i have taken 65shots of depo and burly a week ago i took my 6 shot , and sents i have been takeing it i have not had any trube only when they found a lil bit liquid in my right side but took pills know its better, but now i have been having this problem where i dnt feel when i need to pee, like i yusto know i just get lil accidents or i feel somthing wet , but i dnt pee a lil bit i pee i fell like i pee like a galon. and all this just pappend when i took my 6shot . is this nad what can i take or do to be bk to me my normal self.. plez plez help me
Hi Lizzie – I recommend Fertility Awareness along with your condoms. No need for contraceptive hormones or gadgets at all when you learn to identify your fertile times. You can learn to chart your cycles at http://www.justisse-chartng-app.com or perhaps there is a local teacher in your area.
I had 1x depo shot in Feb and within 24 hours felt terrible, I literally slept most of 2 weeks and when I was awake and at work I could barely function I was so tired, and very irritable. I had a heavy period 9 weeks after the shot and decided then I wasn’t going back for a 2nd go. A couple of weeks after the shot was due I started feeling better, then had a couple of weeks where my boobs were so sore I could only just get my bra on, then I went through a much better phase, not as tired or weepy or irritable and lost all of the previous bloating. Unfortunately this hasn’t lasted and I feel like I’m back on the dep cycle, am bloated very tired and irritable.
I have been reading Dr John Lees books and think I may need natural progesterone to help balance me out of this cycling phase the only problem is I’m in the ME and have no access to a decent dr, am travelling back to the uk next month for a couple of weeks and struggling to locate a Dr following john lees philosophy; any recommendations would be so welcome.
Hi.on january I was diagnosed with endometriosis. And to get rid of the cyst my doc prescribed depo.i had a shot everymonth…I havent had my periods since after the first shot.almost 5 mnths..now im having small spottings of blood…and its v difficult,because in near future I wud very much like to be pregnant.can u pls tell me hw long the effects will last and why spotting is there?? Thanks
I have been on Depo Provera for more than seven years, recommended by my doctor to treat my severe and debilitating periods. I have found Depo to be my “miracle cure,” after bleeding (only slightly) for the first nine months. I was more than willing to endure the bleeding, since the pain, vomiting and uncontrollable urination and bowl movements were much, MUCH worse than light spotting.
Unfortunately, I am now 35 years old, have gained at least 30 pounds over the last seven years, and am having severe cystic acne that is not responding to any treatments my doctors have tried over the last six plus months. They have recommended that I discontinue the Depo, saying it is causing increased androgen levels, therefore contributing to (if not causing) the cystic acne.
My fear is that the horrible, severe, life altering periods will return. Do you have any information regarding the stop of Depo when it has been administered for this long? Any recommendations or suggestions on how to avoid this? I am literally in a panic, and very hesitant to stop the Depo, although any methods that will prevent the constant explosions on my face seem tempting.
I also fear that I may gain even more weight when I discontinue the Depo – are you aware of whether this is true? Unfortunately, I only have two weeks to make my decision.
Hi Cari, Every women’s experience will be different coming off Depo-Provera. Please read this post carefully so you will know what you might experience when you stop the drug. If you do experience heavy bleeding post-Depo, you may want to consider Cyclic Progesterone Therapy as it is explained in this post by Dr. Prior.
Also, you may find this explanation about painful periods from the Centre for Menstrual Cycle and Ovulation Research helpful:
https://www.cemcor.ubc.ca/resources/painful-periods
You are bound to experience hormonal fluctuations, including high estrogen and low progesterone levels post-Depo. The reason for this is explained in this post. This may lead to a return of your symptoms for awhile, so the goal will be to work through this hormonal imbalance to restore normal, ovulatory menstrual cycle function. There are several suggestions in this post that address your concerns about heavy bleeding, weight gain, and acne.
You can download this post in PDF form for future reference here:
https://menstruationresearch.org/wp-content/uploads/2013/04/Stopping_Depo-Provera_Adverse-Effects.pdf
There is a way back to healthy menstrual cycle function but it will take time, patience, and support. I wish you all the best.
Hi ive been on depo for almost 6 years and I am planning on leaving it so I can get pregnant how long should I wait after leaving the depo before we start trying for another baby, do not want to experience a miss carriage
. Is there any connection between depo and miss carriages?
I recently wrote on here about my period starting about 2 months after I got off the shot. I had a normal period and ended about a week after starting. But about 3 days later I started my job as a gym coach and started bleeding again. Is this normal due to the shot? Or should I get it checked out?
I took the shot only once but stopped because I have not stopped bleeding since. From Feb-July. Please help.
That happened to me before last year, I bled for 6 months straight on my first shot and I never got a shot again, until 2 weeks ago. This time my doctor gave me the shot, the morning my period was suppose to come. I haven’t gotten my period since. No other side effects either! Im actually happy, I tried depo again.
Laura is right; read the original article carefully and pay attention to the comments from her, Dr Prior, and me [Lisa]. Click on the links. There’s a lot of good info in this thread, and hopefully enough reassurance. In spite of all the talk of side effects here, most women do recover from hormonal drugs over time, and quicker with a healthy diet and lifestyle. Some need extra support; hormone balancing, repairing the gut. If you are systematic and optimistic, you will get better.
I was on depo for 3-5 months and I ended up getting pregnant… but I didnt realize it because before I knew it the shot killed it… I got off as soon as I could and I refuse to use it again!
March 5, 2014 i got the depo shot. About ten days later i started my period, even though it had ended the day before the shot. Now July 7, still bleeding. After going to the doctor i was told to just wait it out. When this started it was heavy like the worst part of a normal cycle… it has since gotten extreme and there are rather large clots. Should i be seeking a different doctor or just do as he says and wait this out?
I have been on the shot since 2008. I never had a period, rarely see even has spotting. I didn’t have cramps either, so I thought the shot was ideal. This past winter I started experiencing extremely painful cramps, random bleeding, low back pain, and extreme pain and bleeding after sex. The doctor told me he thought it was because the lining if my uterus was so thin from low estrogen from the shot. I decided to come off the shot since it was causing these problems AND I am hoping to get pregnant within the next year. My last shot was in February, so by May it had started to leave my system. I have noticed an increase in nausea and bloating, which I can deal with for the time being. What is causing me major anxiety is the weight gain. I work very hard to maintain my weight, I eat very well and exercise 5-6 days a week. I am getting married in 2 months, and I have already put on 5 lbs, despite INCREASING my exercise routine and getting a little bit more strict on my diet (in hopes of losing a few lbs by my wedding). Instead I continue to gain weight and have ridiculous bloating. I am nervous about fitting into my dress, never mind feeling extremely uncomfortable in a bikini on te beach on my honeymoon! After reading this article, it sounds like I’m pretty much just doomed to gain weight steadily until I start ovulating again. Is there anything that can be done to help these symptoms? I have IBS and several other digestive issues, so I’m actually kind of used to being nauseous and bloated all the time, but this has taken it to a new level. Should I take some sort of progesterone supplement to balance out my hormones?
Thank you for your response! I am starting to see some progress in my symptoms now.
My experience was similar to yours, and I hate to be the bearer of bad news but I gained 30 pounds in four months once my last shot wore off. Same as you I eat well and excercise consistently, plus I’m 29 and I’ve always been around the same weight plus or minus 5 pounds. I tried dieting and I still gained weight. I also have IBS believed to be because of the shot. It’s now been 10 months since my last depo shot, and my weight has stabilized so at least I’m not gaining anymore (though I’m still 30 pounds overweight), and I may possibly be starting to be able to lose weight. I also bled for 3 months straight starting in March and had horrible cramps, it seems to possibly be tapering off though. I am a newlywed too, we were married in September, this has made for a miserable newlywed experience. We wanted to start trying for children last month but with the bleeding obviously it isn’t going to happen until that stops. I got a new OBGYN that is awesome, he said he refuses to prescribe depo because my experience in his opinion coming off depo is not uncommon. He thinks it’s likely that in August, a year after my last shot, I will start being more normal. He explained that since depo is an oil based injection it takes forever to flush it out of your system and these symptoms persist until it’s gone. He said there isn’t much of a way to speed up the process (though I have a friend that’s into herbs and I’m doing blood and liver herbal cleanses to see if that helps), but testing your hormones and taking hormones specific to what you need can help ease the symptoms. I am also taking herbs that help with hormone regulation. You can find that stuff at natural food stores and an employee should be able to help you find what you want. Good luck! My doctor did say I have had an exceptionally bad reaction to this, so maybe your symptoms won’t be as intense.
I am 51 years old and was on the shot for 21 years. My doctor stopped giving me the shot due to my age. The last injection I received was in Dec 2013. I have had several periods since March with no issues other than they are not at the same intervals or for the same amount of time. My biggest issue is the weight gain. I have gained 20 lbs since March. I have not changed my eating habits, but I still keep gaining weight. What is the possibility of having a thyroid problem caused by the shot?
My mom made me get off the pill and start taking the depo provera shot once we found out my bestfriend was pregnant. My mom did not want grandkids and ive been in a long term relationship . I am 16 years old and in December of 2013 my mom had me go get the shot. She did not take me mystepdad did. I cried so much as I was getting the shot which my mom told me It would be in my arm so I was in complete shock when they told me to drop my pants. When I got the shot I weighed 105 pounds. As you know when you get the shot your suppose to gain weight and your not suppose to have a period. Just about 3 weeks later I weighed 84 pounds and had uncontrollable bleeding. I went back to the doctor they said start taking the pill again and your bleeding should stop and we will not continue doing the shot. The pill has done nothing. From december 2013 – may 2014 I was on my period. All day everyday. And the cramps never stopped. I just got so use to having cramps I dont feel them anymore. I had not been able to gain weight. I throw up almost everyday . I never have an appetite. If it waznt for weed I would probably be dead because that is the only thing that helps me eat. I have to get my medical marijuana card when im 18 to save my life. Since may of 2014 to now “july 2014” I still bleed . Not everyday about every 2 days. And then one week out of the month I bleed everyday as if a normal period. But the point is I still bleed almost everyday . Im now 17 and Ive gained about 2 or 3 pounds I weigh about 87. Ive never felt so ugly. I get made fun of everyday now for my weight. I use to feel so beAutiful. I dropped 3 pant sizes… I cant even fit into a size 0 none of my clothes fit and I caN never find anything that fits me. I cant eat I throw up I bleed all the time ive gotten use to the cramps I feel ugly im always dizzy nautious . Its been almost 8 months. The doctors have done nothing and neither has my mom. It feels like im dieng everyday . Thank god for marijuana . Its saved my life . Please listen to me and spread the word. I wouldnt wish this to happen to anyone not even my worst enemy. God bless.
I am a 40 yr old woman with endometriosis. My endocrinologist/gyn prescribed depo because by not menstruating, my endometriosis stay in check. And it really has helped in that regard. However it has been over 2 years and I’ve been considering an alternative because of the bone loss side effect. Further, I’m fairly sure I’m beginning perimenopause because of the cystic acne I have been experiencing and general mental fogginess.
However this blog is terrifying me. I really frightened to switch birth control treatments. Do you have some advice?
I was on Depo for over 5 years. I broke my elbow and had two surgeries so I missed a shot and decided to go ahead and come off of it, since I am almost 47 years old. I did have two broken bones this year, so that kind of worried me. I feel I have been gaining and gaining the last two months, its been since April. I have a son with type 1 diabetes and a husband with type 2, so we don’t really eat a lot and watch our carbs. I run (jog fast) but the weight just sits. My breasts are swollen and hurt, my stomach is bloated and I actually WISH for a period, so maybe it will kick me back into gear.
I was on Depo for over 5 years. I broke my elbow and had two surgeries so I missed a shot and decided to go ahead and come off of it, since I am almost 47 years old. I did have two broken bones this year, so that kind of worried me. I feel I have been gaining and gaining the last two months, its been since April. I have a son with type 1 diabetes and a husband with type 2, so we don’t really eat a lot and watch our carbs. I run (jog fast) but the weight just sits. My breasts are swollen and hurt, my stomach is bloated and I actually WISH for a period, so maybe it will kick me back into gear. If anyone has suggestions on how to feel better, please let me know. vitamins? types of fruit/veggies?
Hi there,
I had my first depo shot in April of this year. Days later I felt terrible and told my doctor, and was told that all I could do was wait it out and skip the next shot. In early June I had my first period (only lasted 10 days) and skipped my second shot. It has been a little over a month since then and I am experiencing sore nipples, heartburn, backache, and weightgain.
My question is, when is it a good time to ask for those hormone replacement pills? I’ve had a terrible experience since that needle went in my arm! I just want my body back. Is there any vitamins I could take to help my body along?
About me: 23, want a baby in less than or up to 24 months time
I was on the shot for 4 years and stopped about 3 months ago and i am having massive abdominal cramps but to blood..hope thats not too out of the ordinary. And i used to weigh 112 pouns but as soon as i started the shot ive gained a ton of weight cuz now i weigh 180 pounds but i enjoyed the no periods.
Hey guys..I am 37 and took my 1st shot of depo on March 28th 2014. I got some bleeding for about 10 days in May. I had to take another shot on June 28th but I have decided not to continue with this as I have gained 10 kgs weight. Is it important to continue with the shots once you have taken ? I also want to know when am I likely to get my periods and return to normal cycle ? I still haven’t got my periods and I am really worried. I also want to know, should I start taking contraceptive pills since the effect of depo must have worn off a month ago. But I don’t know if I have to take pills then when and how do I start !! Because normally pills are recommended to be started from the 4th day of the period and I haven’t got them until now…plz help as I am really worried.
I finished taking depo provera about 1-1/2 years go at the suggestion of my doctor regarding my inevitable approach to peri menopause. My mother had a hysterectomy after I was born so there was no evidence of what my likely menopausal course would be except from my sister. My sister, 52 now, had just started night sweats and hot flashes about her 50th birthday so the thought was I needed to be off depo before that. To be safe, I came off at 46.
I had some breakthrough bleeding in the last year and a half but no real period until this month and WOW! My cycles were never crazy heavy when I was a teen / young adult. I was never crampy, or moody. Often times it was a surprise when it came on. I never had a desire to get pregnant and really was happy when I heard about depo in my late 30s. No period? Yes, please! We did the bone density tests and monitored my symptoms and since I was asymptomatic and bone density testing was not concerning I stayed on depo for almost 8 years.
My ‘first’ period is now in its 8th day with no signs of stopping. The stories of months scared me a bit but my sister, who was never on depo has been menstruating for almost 6 months because of the perimenause so I’m glad Dr. Prior mentioned that it was a typical symptom of perimenause and not just coming off depo, I am now getting night sweats and hot flashes.
Anyway, I just wanted to say THANK YOU! This article has calmed my nerves. I’ll wait another few days and if it’s still not slowing I’ll go get some ibuprofen and schedule an appointment with my doctor for hormone shots. I guess I was expecting sparkles and a balloon, at least, welcoming me into menopause but instead it’s pretty much as it was when I was 12 and got my first period.
Where do you get your shot? I have no evidence other than personal experience but I typically got my shot in my gluteus muscle but a few times the nurse has insisted it be in my arm. After a few times of experiencing exactly what you described I wouldn’t let them do it in my arm again and never had those symptoms when it was in my butt. I thought that maybe it was the uptake of it. Less muscle /fat in my arms so flooded my body faster but like I said, I have nothing except personal experience.
I’ll start off by saying this is the most informational blog I have read and I’m hoping someone has some helpful insight for me.
I started depo when I was 19 in 08/2007 because I went to the Dr with heavy periods which included what I called meat chunks. They told me I was losing too much of my uterine lining and also did a transvaginal ultrasound which showed I had a small cyst on one of my ovary. The Dr decided I needed to go on Depo, which was fine with me as long as it stopped the problems.
On depo I gained 30lbs. In 2012, I decided to get healthy (balanced diet with vegetables and whole grain) and lost all of it and got back to a health BMI. My last Depo shot was May 2013, because my husband and I would like to start a family. I started working out harder to “sweat” the depo out of my system faster and consumed lots of water. I gained 10lbs back regardless of the extra workouts. Oct-Nov of 2013 my breasts were extremely tender! One day I woke up at the end of Nov and the breast pain was gone but I was extremely emotional.
No periods until Feb 14. When that happened I had cycles every 10-14 days and they were heavy and painful. I recorded my fertility out of optimism and on day 8 of my cycles I was “ovulating” according to the ovulation test. After 3 months of bleeding that often/much I went to the doctor because I was getting extremely tired. She put me on a 10 day progesterone pill. It didn’t stop the short cycles as I was bleeding again on the 10th day of the pill. She sent me on to a gynecologist who did another transvaginal ultrasound.
He didn’t have much to tell me besides I hadn’t been ovulating at all. I had 5 follicles on my 1 ovary that day and I had “fluid above my cervix” He didn’t have any help for me either (kind of felt shunned for using Depo) and told me to wait it out or he’d put me on Clomid. (which I don’t want!)
For the last 2 months I had extremely light periods. (no cramps, mostly clear fluid with a little red) This month my cycle hasn’t come at all, but I have a lot of clear/white fluid down there. It’s been 50 days since my last period in June. I’d like to be “normal” before we start trying to conceive to ensure I’m healthy enough to carry. Have I stopped cycling all together? What is going on? I already eat healthy and exercise, so what other options do I have besides clomid? My husband and I wanted to start trying in August, but I’m scared to with all these inconsistencies and fear of multiples with clomid.
Could the clear fluid “down there” be cervical mucus? Perhaps you’re trying to ovulate. Clear or cloudy discharge is a sign of fertility and indicates high estrogen levels related to ovulation. Wouldnt it be nice to know that your cycles are returning? I suggest you get back to charting and study more on mucus observations. chart as much detail as possible (moods, energy, libido, as well as discharge and temps.0 this info will be helpful in diagnosing your return to fertility. best of luck – Lisa
Plz I have had 3 shots, i blended for long, sometimes 3 weeks in a month I met my doctor and he gave me an injection to correct it now I havnt seen my period for over 2 months and am worried Plz help me
Firstly, please don’t be worried. As this post explains, coming off Depo comes with a range of experiences, and return to normal cycles will vary from woman to woman depending on age, your cycles before Depo, and your overall health. At 37, your body may be having a hard time reasserting normal hormonal function.
You don’t mention what contraceptive method you used before Depo or why you chose to take Depo, or if you still want to have children. All of these factors come into play in making an alternative decision after quitting Depo. If you were experiencing problem cycles, there are other ways to manage things like heavy bleeding or irregularity. You can search these topics at http://www.cemcor.ubc.ca to learn about treatment options that don’t include hormonal contraception.
In choosing an alternative birth control method you must first consider if you want to continue with hormonal methods or switch to a non-hormonal method such as copper IUD, condoms, or other barrier methods. A Mirena IUD, which releases a different progestin than Depo and in a much different way, may be a suitable option for you.
I had my first depo shot at the end of may 2014, i’ve not bled at all during this time, but I have gained 8lbs since taking the shot. I’ve decided not to get the 2nd shot because of the weight gain.
Over the last week I’ve been experiencing nausea, dizziness, sleepless nights and mild stomach cramps, flu like symptoms, I have also being going for a pee about every hour! which isn’t normal for me! I am wondering if these are all side affects of comming off the jag, by looking at some of the posts on this page it sounds like it could be. Am hoping these issues will pass quickly and I can the weight off and get back to normal! Stacey
we all hope you recover quickly, too Stacey.
Eat healthy, get exercise, rest and sleep. Be observant, make note on how you’re feeling and why you bleed. I hope it all unfolds smoothly for you.
I been on this drug for 4 year now I hv stoped and god I my going thru hell no periods .I hv a killer hot flashes night sweats my docter says im going thru a early menopause im 35 still wants kids very disappointed. I been off depo shot for over a year now the first few months I a had my periods but they were I regular. ANY HELP WHAT TO USE MY DOCTER SAYS THERE IS NO CURE FOR THIS….
Help me please I need to kno what or if there is anything to help me feel better after stopping the depo shot … I feel sick sore depressed and like giving up on life
I got my first Depo shot 2 months ago. Every since I got the shot I’ve been bleeding It’s like a light period. I think 2 months of bleeding is way too long has this happened to anybody else?
Thanks for the posts. They are very helpful as I’m currently trying to stop taking Depo for my endometriosis.
I have been on depo-provera for 10 years and am stopping the shots this week. I am highly allergic to ibuprofen (I carry an epi-pen just in case I am exposed to anything with salycilic acid). I am worried about what I am hearing regarding coming off of depo-provera and before going on, I used to have heavy, painful periods. Is there something else that I can take for pain? Tylenol doesn’t help at all. Thank you!
Joanna – do read the interview with Jerilyn Prior, there is some excellent material about hormones that will give you insight into what could happen. Regardless, dont assume there will be probs. Get healthy, eat well, be active, and do things to calm inflammation in general thruout your body. People with allergies and pain tend to be big inflammation factories in general. Look for ways to quench the fire; tai chi, pineapple, supplements like tumeric – whatever works for you. Lisa – an optimistic herbalist
Yeni,
I had very bad joint pain in my ankles, shoulders & wrists. My last shot was March 2014 and my period has just returned with a vengeance bug I am finally feeling like my old self again. I hope your symptoms are easing, good luck
Yeni,
I had very bad joint pain in my ankles, shoulders & wrists. My last shot was March 2014 and my period has just returned with a vengeance but I am finally feeling like my old self again. I hope your symptoms are easing, good luck
I just wanted to write an update that may give some of you hope. So my last Depo shot was in November 2012, after no period until July/August 2013, nonstop heavy bleeding since then til November 2013, then cycles (25-33 days) with up to 3 weeks of bleeding (brown blood, clots, bright red, you name it, I had it)until my last period end of July 2014. Well, feeling completely fed up and feeling like my system is broken, I made ANOTHER appointment with womens clinic to ask why am I, almost 2 years after shot, still all over the place with cycles/periods/moods. I was advised to wait 2 more months then if cycles still not better I would need to have a coposcopy and treatment as she wondered if I have abnormal cells on cervix (even though nothing has ever come up in papsmere). Well, 2 and 1/2 weeks after that appointment discussing a possible coposcopy, I realised for the first time I have not started bleeding. I have been so used to bleeding more days than not during my cycle that this was very strange. Plus I have been having pregnancy symptoms (but I just thought they were pre-menstrual symptoms). So, took a few pregnancy tests and they are coming back as faint positives. I will have a blood test in 2 days to confirm the positive, but I am so happy and shocked. Almost 2 years after last Depo shot and a horrendous roller coaster ride of non-stop bleeding/no periods/mood swings/depression, somehow I am pregnant. So, please, don’t lose hope! I’m hoping that this will be a healthy pregnancy and that the Depo hasnt messed up my system so much that I miscarry. Thinking positive!
Hi I had a question about depo to I got off depo June 24 of this year
I had bleeding in July which I thought was my period anout 4 days later it stopped it wasn’t heavy was just barely enough to get on my underwear
I went about a week and it started again this time lastin for about six days now this morning I’m bleeding again it’s only been about two weeks since I bled last time.
Is this effects of depo or is something wrong? They’re not ever heavy just enough to barely get on my underwear.
Btw
I was on depo for six years.
follow up….sad news unfortunately. I had my blood test for HCG and the results were less than 5mil HCG, which means no longer pregnant. The doctor says I was pregnant, but for whatever reason, have had a chemical pregnancy (early miscarriage). I am sad that the pregnancy did not work out (sorry if I gave anyone false hope), but so so happy to know that I am able to conceive. I truly did not know if I would ever conceive after the havoc Depo has wrecked on my body and cycles. So, will keep trying.
Who’s been following this thread? More than a miscarriage story:
L. Faye says:
September 2, 2014 at 2:55 am
follow up….sad news unfortunately. I had my blood test for HCG and the results were less than 5mil HCG, which means no longer pregnant. The doctor says I was pregnant, but for whatever reason, have had a chemical pregnancy (early miscarriage). I am sad that the pregnancy did not work out (sorry if I gave anyone false hope), but so so happy to know that I am able to conceive. I truly did not know if I would ever conceive after the havoc Depo has wrecked on my body and cycles. So, will keep trying.
I say:
She’s right to focus on the conception. We have learned that she ovulated. Also that her hormones are trying to talk to each other. Perhaps her fertility is returning. I recall other signs of it in her story (normal periods lately). She is not out of the woods, however, and a pregnancy may have had higher risk of complications (glucose, cardio, gall bladder). Nutritional levels (folic acid, iodine, etc. can play a role in how quick we recover our fertility.
I say this gives her more time to become better nourished and get some healthy cycles behind her. The ovary has been in limbo and has to relearn how to produce eggs again, so one of the 1st few eggs might have been blighted. Also in limbo was the endometrium; made inhospitable for implantation and now relearning how to build up and shed out properly.
I urge L. Faye to go on a health kick and chart everything. There’s nothin more reassuring than watching a few normal-ish cycles unfold in one’s own handwriting.
My last shot was January 13th, 7 and a half months ago, I have yet to start bleeding again, gained 30lbs in the last 5 months though I’ve been eating less and more active. The last month and a half I’ve been overly sensitive, often have terrible cramps, sensitive skin (I don’t want to be touched), the worst mood swings I have ever experienced (I started depo because my PMS was so bad I’d miss work) my sex drive is shot, hot flashes and night sweats… And I’m only 24! I just spent Saturday yelling in an argument with my sister over a mirror, a mirror! And then I spent the day crying. I drink an insane amount of water, eat healthy… I don’t understand. I wish I never would’ve started on depot..
Thank you Lisa. I appreciate you looking over my ‘history’ and your advice. I will definitely work on eating healthy and keeping up with fitness and letting my body recover over the next month or so. I have been charting EVERYTHING (heavy/light period bleed, clots/no clots, crampy, tired,moody,unprotected/protected sex, etc..)over the last 3 months and it has proved very beneficial. Especially during hospital/doctor visits. I would encourage anyone coming off Depo or trying to conceive to do the same. I only wish I had started doing it earlier. I will keep you posted on my ‘situation’. Thank you for the support.
hey Laura and Dr. prior, I’m 21 and I’ve been on the depo since march 7, 2012 (my lil girl was born on the 4th, 3 days before) and I bleed for mths and myths and the docs were even telling me that it was my uterus thinning out it’ll get better. well it never did, sorta. me and my husband and our lil girl now 2 years old, we’ve talked bout having another! but, I can’t stop bleeding in order to have intercourse with out thinking omg! am I gonna bleed? I stopped taking the depo in Feb. 2014 it was my last shot, and ever since I’ve been having 2 periods each mnth and they last bout 6 days, in the beginning and near the end of each. before the depo my periods lasted like 3-4 days gosh I loved it! lol, and I had trouble gaining weight on the depo, but now that I’m not taking it, I’m gaining weight quick, I’m eating like I’ve always ha’ve, alot!! except I’m gaining all of it instead of burning some. anyways all these symptoms bleeding, weight gain, bloating, enlargement of breasts, pregnant related ssickness(like you got butterflys flying around), mood swings, easily irratatided, in stage 2 of having cervical cancer if pap smears are not up to date, means every year now, they told me that September of 2012, etc.. started increasing like within the past month, and it’s scary, I’ve been reading the post and some help but most hasn’t related to my problems and answers. why am I bleeding 2x a month? have I become sterile (not able to have anymore children)? is there any way I could be pregnant? was something not fixed or became non-usable after having my first child? am I getting better? worse? did I make a huge mistake considering the depo? I need your advice and your own opinion, as if you were not a doctor, if you were me, what would you do? now tell me as being a doctor, what would you do? what is going on with me? please respond soon!! thank you! -katelyn and jesse and aubrianna
‘… so is that your opinion? I don’t get it.
Hi, a little late but I just discovered this website. I’ve been on Depo for about two weeks now and I’m experiencing terrible side effects every day. Most of them are common, like depression, nausea, fever, acne, fatigue, and headaches, but lately I’ve been experiencing odd symptoms. I looked them up on the side effect section on drugs.com but they’re less common. I have been experiencing insomnia, trouble swallowing, panic attacks, skin rashes, increased thirst, nervousness, and chest pains. I might just be a worst case scenario, but this is making my life miserable. I just want to know if other people have experienced this and if it gets better. And also it seems like every day I develop a new side effect.
Rachel (Sept 4, 2014) reports side effects right away after her 1st depo shot. I call people like her “canaries in the coal mine”. (Miners used to take birds down with them knowing they’d exhibit illness if the air quality became tainted before the workers were harmed.) Those people who react right away warn the rest of us that we really are exposing ourselves to something toxic even if we seem to be tolerating it OK so far.
I have been on the shot now for two years. I was turning 16 and my mom made me, I am now 18. After ive read and saw all the comments im thinking it was a good idea coming off the shot. But I am experiencing horrific after affects. I wake up in the morning with my stomach so upset that when someone coughs it makes me gag. In the past few days ive been really scared because my nipples started hurting and then my whole boobs. I was really scared so I got on the internet and found this site. After reading the symptoms of everyone else I have been experiencing a lot of things that I honestly didn’t pay attention to until I thought back after reading this. I think when a child gets on a birth control they should be able to choose. I AM ABSOLUTLY MISERABLE! ugh!
Hi, I’m 23 and have been on the depo shot for roughly 5/6 years as it suited my lifestyle and body. (Used to suffer horrendous acne, periods,cramps,nausea etc…) I came off the shot just over a month ago and left the last month hormone contraceptive free… Due to starting a new job soon my partner and I decided I would go onto the contraceptive pill so to cover ourselves whilst I get settled in my new job and to avoid any pregnancy. (I would love children and actually aspire to it however I would like to settle in my new job first!)
I started the pill 3 days ago and yesterday I finished work with the worst pain in my thighs, almost like growing pains however somehow much more intense, that night in bed I got around 3 hours maximum sleep. For some reason I just couldn’t sleep, then I was jumping from being freezing cold to hot flushes and being drenched in sweat.
My breasts and nipples have been hurting for little over a week now however that I can handle, I figured I’d have some symptoms to show for the switch. I’m currently just concerned about the hot flushes during the night as I genuinely think my worst nightmare would be to be experiencing early signs of the menopause.
I haven’t bled entirelly however there has been a lightish brown discharge from downstairs.
Id love some advice, I know it’s not been long and I’m impatient but I’d like to know what I’m dealing with.
Hi
ive been off the depo since may 2013 and still havent had a period, its very frustrating as trying for a baby, docs said come back jan 13 to be given something to start my periods but when I went back changed there mind and said come back may13, then again changed there mind and told me to wait 18 months if nothing has happened, very upsetting.
Sorry replied to wrong post but think you only have to wait 2 wks providing you have a pregnancy test which is neg
Obviously I’m not in a terrible situation cause no one responded to my questions.. Aw well, I’m on the verge of suing the depo and my doctors!!
Hello Katelyn,
I don’t profess to be an expert on these matters other than my own personal experience and my current academic studies but firstly I would say that you really need to try to not get too stressed about your current issues. Stress makes everything worse. Secondly, for reassurance, I had all of the symptoms you are experiencing plus panic attacks and suicidal thoughts when I was coming off the depo, but they do pass. My one bit of advice (which I myself received from my doctor) would be, forget about all hormonal contraception for now. Of course you mention yourself and your partner don’t want children, neither do I (I’m 22) and quite honestly if this is how you both feel then your boyfriend should understand your current predicament and take some responsibility; use condoms.
As frustrating as your current situation is, you are young (like me) and you need to remember that your body is in it’s prime and what you are experiencing is a readjustment of your natural sex hormones. If you look at yourself as an animal, remember that we are solely designed to reproduce. If you are healthy and look after yourself, your body will do the rest. It’s unpleasant whilst it’s going on, but really, it’s very impressive. Please don’t worry too much.
Kaetlyn, I’m sorry you are feeling confused and scared by the adverse effects you are experiencing from stopping Depo-Provera. Other than the explanations offered in this post, and Lisa Leger’s advice to go on a “health kick” (eat well, exercise regularly) and charting your cycle events and other observations ( as L. Faye notes in her comment on September 2), I can only suggest that you hang in there while your body works hard to sort out your hormonal ebbs and flows. If you want your body to return to normal menstrual cycle function, avoid other hormonal contraceptives.
One thing that concerns me is how many women have commented, both on this post and my other post about coming off Depo, that they are not having protected sex after stopping Depo. If your intention is not to get pregnant, then be sure to use condoms as an alternative method. If you do wish to become pregnant but are experiencing erratic cycles, ongoing bleeding problems, etc. it may also be a healthier choice to wait until your cycle returns to some sense of normalcy before attempting a pregnancy. If you do wish to become pregnant, you may want to consider asking your doctor for Cyclic Progesterone Therapy, explained in this post, to help you achieve regular ovulatory cycles.
All the best.
I am thinking of coming off the depo injection I am 53 years old and have been on it for 26 years but a little worried now about all the comments
thank you Lizzie for that kind and reassuring comment to katelyn. You’re quite right to point out that we are mammals and our bodies are designed to repair and be healthy and strong. All we need is healthy food, exercise, rest, love, fresh air, clean water, sane living arrangements and so forth. Most importantly, we need to Stop Fukkin Around With Our Hormones and Leave Our Cycles Alone to Unfold Naturally. nuf said – lisa
Hi everyone! I am really just confused I would usually have a short 3 day period… This is my first time taking the shot and I already have 5 days on my period and I keep thinking it’s going to go away but no, I just continue spotting! Please anyone, with a similar experience like mine?
I took the depo the day before my bday sept 16. I was fine all day then when i woke up sept 17 i was in such sever pain…i forced myself to go to work but when i came home i couldnt take the pain anymore and went to the er. I was bent over inpain and just bawling. My stomach hurt so bad. All i got was a loratab and the doc telling me the depo is different for every woman. When i saw my ob the following day, still in pain, she did a sono and said everything was good and didnt think it was the depo. Ive had the pains in my stomach ever since i took t the shot. I know its from the depo. I read the side affects, its one of them. Will it ever go away? I have the pains every day. Not as severe as that first day but still in pain.
Hi,
I received the depo provera shot in mid May of 2013. I received 2 shots in total. Officially my depo was ‘done’ at the beginning of Nov/mid-Nov 2013. I weighed about 115 at 5’6″(normally I was about 120-125, a bit thin at the time). I stayed this weight until about the beginning of Feb 2014. At that point I gained about 13-15 in two weeks. It really just came out of nowhere. I have continues to gain a bit of weight until now (September 2014) I weigh about 134. My weight does not really budge, I can go up and down a few lbs but no matter how good I eat/exercise I cannot loose the extra fat I have put on. I am still very fit and have good muscle (I have always been active and athletic) under the fat. The fat is just being stored mainly on my thighs, butt, hips and stomach. It is a combination of fat and bloating that doesn’t seem to go away with any effort I make. I have been extremely fatigued since I gained the weight, unfocused, it has been such a major change from my normal self and very scary. I have good optimism that with more major lifestyle changes and time I can get this all out of my system. I also realized looking back that my second shot had caused numbness in my lower right leg for a few weeks. I also had a large swollen spot on my leg in Feb 2014 right before I gained the weight. I seem to have suffered from a lot of the side effects that this drug can cause without knowing it. I have truly learned a lesson in putting things in my body that change the natural habits your body should go through and doing my research too. I consulted a homeopathic woman who did assist me through herbal medicine to get my period once in the middle of Aug 2014, however I have not had a second period and it has been about 40 days since I had it. I know I am starting to get back on track, but this has been a long and depressing process. I wanted to share my experience so far in case it helps anyone else.
I also wanted to ask the doctor that if I were to take the cyclic progesterone therapy, will this help get me back on track and is it natural? I really would like to take the natural route only. Please advise.
Thank you for all your advice and comments. It’s helpful to know I am not alone.
Kandace
Thank you so much, Anne RF, for responding, and thank you Lisa, too, for all of your input, along with the other posters. I came back here with an update, late August I finally did get my period (finally!!!). I guess beggars can’t be choosers, but “holy h-e-double hockey sticks” this pain is pretty darn bad. I will be detailed, since we’re women here, and I hope it’ll help someone else who might go through this. I woke up out of a solid sleep feeling like my left ovary was simultaneously being stabbed and on fire, and then it felt like my fallopian tube decided to do the “wave” and the rest of my system went into contractions that were so strong and painful, I literally couldn’t move for about ten minutes or even get up the strength to walk to the kitchen and rummage for the ibuprofen. It was bad. On par with the worst period pain I’ve ever had when I was a teenager, probably worse. I mean, closest I can compare it to is when I was in early stages of labor with my daughter. I felt bloated, my uterus was a fluid-filled balloon, and like I was going to give birth (to what, I wondered, not exactly like that’s the situation, but feels eerily similar to that or miscarriage). Now, it also was not like a normal period because the pain was intermittent. I would have it for an hour and then it would disappear for a few hours (without meds), and I’d think it was over, only to be awakened in the middle of the night (like, now), and have it reappear. I bled for four days the first time, it started off like a normal period, and then got really heavy. I’ve had my “period” three times in the past four weeks, for about four days at a time, second time was a few days after the first time was over (I thought), and then I started bleeding various shades of black, bright red, and light pink, with no rhyme or reason. It went away a few days, and started again, this morning, with a vengeance. Now, it was actually so bad today, that ibuprofen wasn’t touching the pain, and even with a serious pain killer I can still feel these cramps, which go from the front uterine area (mostly on left side) all the way to my back. And it started *this* time in my right ovarian region, then the middle, and back to the left side throbbing, again. Never had back pain, before with my periods, until now. I went to the women’s health clinic where I received the shot in this past week, to let my clinician know what was happening, and she sent me to get a pelvic ultrasound, since I was obviously in a lot of pain and had pain issues with the left ovary before going on the shot. I don’t know the results, yet, and won’t for a few days, but she said it could be, “just one of those awful stories of things women experience when getting off of the Depo.” I looked at her, like, “huh?” If I knew there were problems/pain like this when getting off, I would have never taken the shots! 🙂 I’d have to say, going through this tail-end now of the Depo experience, I wouldn’t recommend it. If the side effects weren’t there, maybe, but this just stinks! My sympathy to anyone else going through it, and thanks to the ladies who have been reassuring that they did get their periods again, when I wasn’t sure if mine would come back. Also, thanks to those who say this type of stuff will eventually regulate, thanks for sharing, so we can all find each others’ experiences and talk about this. I did a little reading and saw that some of the extra pain/bleeding and sore breasts (which I have had, too) could be from an overload of estrogen in the system. Isn’t there a chance that could be really bad, if it’s for a while? Are there any estrogen-related cancers to be worried about? Just wondering.
Excess estrogen is a simple way of explaining a more complex process involving liver function and intestinal environment as well as the hormone feedback loop. If anyone is looking for ways to “reduce excess estrogen”, I suggest looking to the organs of elimination. Avoiding constipation is important. You might want to investigate things that help the liver convert estradiol to the safer forms of estrone and estriol like Diindoylmethane (DIM) or Indol-3-Carbonol (I3C). I’ve seen good results in reducing symptoms of estrogen dominance like fibroids, endometriosis, breast pain, heavy menstrual bleeding, and perimenopausal PMS.
I was on Depo for 12 years, and came off about 10 months ago (cold Turkey). I thought I was starting to feel better, but just made a trip to the ER yesterday, nausea, bloating, unbearable. Dr. thought it was my gallbladder, did numerous blood test and gallbladder scan, everything came back normal. I am wondering if this is now menopause, since the Depo should be out of my body…I am so sick of feeling sick!
Tami, I too was on depo for many many years. I am looking for other women have experienced any kind of bone density loss, osteoporosis, frequent fractures, or any other bone loss issues.please let me know if you have experienced any of these other symptoms. And if any other women have experience with these symptoms I would be interested in discussing it further.
If I just stopped my depo shot as of 9/24/14 but have begun taking the generic version of micronor, do you think this will increase my progestrone levels so I do not suffer as much from the post-depo side effects?
Good Question about micronor post depo to mitigate the withdrawl. I hope Dr Prior answers because she’ll be able to explain the strategy she uses and why. (read her comments) From my perspective, it’s still a synthetic hormone and I want everyone off all such, however I do see a temporary role for a drug to treat the side effects (effects) of another drug at times. Ultimately the goal is to have healthy cycles unfolding on their own and then avoid pregnancy using a combo of barriers and fertility awareness, and to treat any irregularities with diet, lifestyle n natural remedies rather than suppressing the endocrine so profoundly with such powerful hormonal drugs.
Hi i have been on the depo shot for 20 years now and never had a period but for 2 weeks now i have does this mean its not working i am 52 and its never happened before i mean its the bloating the cramps and i am not liking it help thanks
does getting off depo make me more fertile and more likely to get pregnant??
i took only one shot of dipo provera and my menses has stopped since. i have being asked to take secure contraceptive to restore my flow. do you think this is helpful and for how long will i continue to remain on secure?
Another update–stopped bleeding, after bleeding on and off for over three weeks, with ibuprofen. Pelvic ultrasound revealed I have a fibroid and a “very active follicle” on my left ovary. My local family health clinic is referring me to a gynecologist to discuss possible treatment.
Hi
My name is Kristena, I have officialy been off of depo for 3 months and 3 weeks. I am currently experiencing sore breast, bloating, nausea and mood swings. Ive been on depo way longer than I should have been. My main concern is, is it possible to get prego immediatkey after getting off depo? I know some woman bodies are different and my bf and i are both curious.
Hi Kristena, The question is do you want to get pregnant? If not, then you should use an alternative birth control method when you stop Depo, probably a barrier if you want to restore natural hormonal function. Although for many women the return to fertility takes months, depending on your health and the amount of time you took Depo, you could get pregnant right away if you don’t use a reliable method of contraception. If you do want to get pregnant, information about how to restore ovulatory cycles is included in this post.
All the best, Laura
I’m 39, and I stopped getting my depo January 2014. It is now October 2014. Just recently for the last 2 months I have felt pukey sick, stomach pains, diarrhea, tired, dehydrated, am getting a period if you want to call it that about 1 to 2 weeks apart from the time the last one ends. I am peeing a lot of blood, but not passing a lot on to a pad. I am now getting dizzy spells.
What is going on as I am NOT pregnant, and all my labs came back great.
I have had the depo shot about 2 times and it weared off and I’m bloated with cramps, spotting a lot, and nausea … I also have had depression for the past week..
Update fron my last post. About 12 days ago, rough guess. I had a period for about 3 days. It returned 2 days ago full force. I don’t know if it’s the side effects of comin off depo after about 14 years of being on it, but my cycle is back full force, stronger than ever, I am tired, loss of appetite, nausea, drinkin too little amount of liquids, and have major cramps, stomach pains, etc. And I feel like I just want to cry or sleep 24/7. And NO I am not pregnant. Are these all side effects? If so how long do they last for?
Hi I was on depo for many years , I gave been off for 8 yrs , my biggest complaint was the sore injection site, weight gain.
I have recently had the extremely sore arm like I used to have when i got the shot ,, I am having trouble lifting , washing dishes, sleeping because I am in pain.
I also have chronic pain and fibromyalgia and often wonder if it is all related //
Susan, I also have had chronic pain, fibro myalgia like symptoms. There have been class action law suits in Canada and New Jersey for women with
bone density issues, osteoarthritis, osteoporosis and frequent fractures. The lawsuits were won in both cases and Pfizer was held responsible for the issues and required to compensate the women. Please look at my previous posts where I have links to the journal articles and news articles about these issues.
Lisa, please read my previous posts about depo lawsuits, timelines & positions on depo by women’s health organizations.
Katelyn, please read ny previous posts on depo lawsuits and time lines regarding depo
Liinda, please read my previous posts with info regarding depo lawsuits and timelines and info on “black box warning” suggesting depo onky be used for 2 years due to bone density issues
where are they located please …. thanks
Here is site
https://www.bigclassaction.com/lawsuit/depo_provera_contraceptive_osteoporosis_class_action.php
I was on Depo for about a year. While on it I had the worst menstrual cycle. I would be off my period for maybe 1 to 2 weeks at a time (why I stopped). I’ve been off the shot roughly 4 to 5 months and I have been having the worst abdominal pain that seems to come and go along with me cycle. The pain starts on my right side near my ovary area and also around my left rib area. At first I though it was a kidney stone but there is no other signs of that being an issue. Could this be the aftermath of the Depo?
I was on Depo for about a year. While on it I had the worst menstrual cycle. I would be off my period for maybe 1 to 2 weeks at a time (why I stopped). I’ve been off the shot roughly 4 to 5 months and I have been having the worst abdominal pain that seems to come and go along with my cycle. The pain starts on my right side near my ovary area and also around my left rib area. At first I though it was a kidney stone but there is no other signs of that being an issue. Could this be the aftermath of the Depo?
I caved under the pressure of coming off my depo. My period had come back after 7-8months of stopping the shot, and imy periods would last a couple days, end, and then have another a week later. Then October I get a heavy, horrible period, the nausea, stomach pains, not eating or drinking liquids, I had enough, and I finally went back on my depo. I have relief now from the stomach pains, nausea, and am drinking more liquids.
I took two depo shots as required by my doctor before having the essure procedure done. This was only my second time ever taking any birth control of any variety. The first time went horribly wrong, as I assume I have a very sensitively balanced body chemistry.
Since having the essure procedure six month ago, I have had continuous bleeding. I’m not talking about mild bleeding… I’m talking about you best buy your tampons at Sam’s by the “flat” bleeding… horrific horror movie bleeding… OMG I seriously think I’m gonna die bleeding.
I’ve been lethargic. I don’t want to leave the house, but if I do leave then I definitely don’t want to see anyone. It takes a series of pep talks, just to convince myself to run the most mundane errand. I am very emotionally sensitive and want to cry frequently. I’m living in this illusion that leads me to believe that everyone is an asshole. I’ve been having panic attacks. I’ve stopped working out.
My boobs are sore, my vagina is sore, and my ass is getting larger. My legs and feet are retaining water. I’ve gained two pounds, but when I look in the mirror I swear it’s 20.
Although I still shower daily and make sure I have good hygiene, I have absolutely zero desire to: brush my hair (literally haven’t in months), wear makeup, wear jewelry, or dress in anything other than jeans or jean shorts and a t-shirt.
Prior to the depo shot, I had a very healthy/high sex drive. Now, I have ZERO desire for sex. I have no desire to date, talk to, or in any way interact with any one.
At this point, my doctor has said “just hang in there” and my body will eventually get back to normal. I feel like I’m going bat shit crazy and honestly don’t care if the rest of my life is spent just me and my yorkie.
Keep reading Marsha – there’s lots of good info. Pay particular attention to what Dr Jerilyn Prior has to say, she knows a lot about this subject and addresses it like an Endocrinologist (which she is).
Hi, I am 24 years old. When I was 23 I stopped pill form birth control because I kept forgetting to take it and I wasn’t having sex. Recently, I went and got the Depo shot as recommended by some doctor. My first shot was in March 2014, Second in June 2014 and then I quit. In March I weighed 158 pounds now (in October) I weigh 210 pounds. You can guess how awful I feel going up 5 pant sizes. I’ve gained all in my ass, thighs, lower belly. I feel tired so I sleep a lot, no motivation, headaches, bones cracking and no period. Ive had lots of stress in the past 3 months but I shouldnt be feeling all of these symptoms. I have read the above comments and I’m wondering if I should continue to wait it out or seek a doctor? I am not currently taking any chemical birth control. Except for what is remaining in my body from the Depo. I wish I was better educated for it.
I regret taking this shot and I feel like a complete idiot for doing it!!
I hope this is a more normal feeling but honestly I hope my body balances out, fast.
Jane, please don’t feel like an idiot. I worked for a family planning clinic as a medical assistance when I got the shot and I didn’t know any better. Depo should be banned. All the symptoms you are having are normal AND so are you. I know it seems like it will never end, but it will. I am putting the link for more info about Depo. Keep writing and read all older blogs and we will all support each other.
https://www.bigclassaction.com/lawsuit/depo_provera_contraceptive_osteoporosis_class_action.php
Valerie,
Thank-You so much for replying. It means a lot to know that I’m not “crazy”.
I enjoyed the article. When do you suppose the weight will balance out and a person can start loosing weight?
Also, generally speaking when can a person regulate their cycles again? I’ve got wicked cramps once a month but nothing to show for. Some articles say 11 months but I’m not sure how true that is. How was these issues for you? Also of note I’ve grown here and there hairs on my face its not that noticeable will that go away?
Thank you again Valerie!!
I started the depo when I was 21 and got off it when I was 24. In total I was on the depo for 3 years. While on the depo I experienced hair loss, hyperpigmentation, headaches, instantaneous crying, weight gain (about 5 pounds every year), vaginal dryness, low sex drive, and sore breasts.
On May 22,2014 I took my last shot.Today is Oct,13,2014 and I’m still experiencing these side effects and some new ones. When the month of September 2014 started, I started to have the New side effects : extremely sore nipples and breasts, my headaches have also come more frequent and more painful, I spotted for about 3 weeks (haven’t had a period in 2 years),Nausea all throughout the day (breakfast, lunch, and dinner times), and mood swings (mostly anger and irritability).
When I read the article and how eating veggies & fruits and exercise will help with the sore breasts/nausea/bloating, I felt doomed. I have been exercising and eating a lot healthier…. but nothing helps. Another thing that is troubling me, is how hard it is to lose the weight that I have put on. When I started the depo I was 115 pounds and a size 5 in pants. Since being on the depo I am currently 130 pounds and a size 9 in pants. I have been eating healthier and exercising 3 times a week every week since the month of August 2014 but have I not been able to lose the weight. I have seen some results but I am no where near where I want to be.
Usually a lot of women are posting when their periods returned.Maybe what would also be extremely helpful is if some of the women could post how long it took for all the side effects to go away and how they battled their different side effects.
Thank You,
Resha
I have been on the shot since I was 16. I lost 20 pounds during my first 2 months. I am now 26 and never been over 110 pounds. I am planning on getting married in April of 2016 and would like to have a child. Would it be safe to get off the shot now, even if I don’t plan on becoming pregnant till after I am marries? And also has anyone ever experienced “WEIGHT LOSS” while on the shot? And if so did you gain after stopping?
Thanks,
Natalie
Hey Jane, I completely understand what you are going through and I have felt and still kind of do feel the same way you do. I gained about 25 pounds from it. The tiredness is one of the worst things. I was and still kind of do get very tired and have zero motivation. I read that Depo can create insulin resistance so your body can’t process sugar. I have been trying to eat fruits and veggies that are low in carbs and eating fish, and other lean proteins. It definitely has helped me avoid being sleepy and regain control over that. My work has suffered a lot from feeling this way. I have been off the shot for 11 months now and still have the weight. I have hope that I will loose the weight and get my body back in balance as it once was. I saw a holistic person and she helped me get my period restarted. I have had it twice, but it’s not regular. My body is definitely working on getting back together.
Well I have been taking the Depo for 5 years now and I stopped in May when I had to receive a double shot due to the fact I had a ‘breakthrough’ according to my doctor; meaning I had excruciating pain feeling like my insides was about to fall out and my vagina was hurting so bad. About a week after that I gained about another 10 pounds and that when I decided I needed a break from this thing. This week I saw my period again for the first time and the pain came along with it. I an monitoring my body’s response for the next couple months to see what happens. My greatest concern is if my Endo will become worst by stopping the shots. At the same time I am planning to take a bone density test to see if there has been any effect on my bones over the years.
Kandace,
I’m not sure where your comment is on here but it had not occurred to me that Depo can create insulin resistance so your body can’t process sugar. It makes sense. I really am annoyed that doctors dont tell you the real consequences of this drug. If I had known what I would be feeling now I would never ever of tried it. I would like to hear updates from you because I was hoping 11 months form now I would be the same 6 months ago.. I have high hopes. I will start to QUIT THE SUGAR!
Kandace, After I wrote you the first time I had an after thought. The doctor told me to go back on birth control and gave me a year prescription of Aviane (apparently the weakest birthcontrol) would that help regulate your period? Of course I didnt take the doctors advice BECAUSE I know my body is weak tolerance for drugs and I dont want more chemicals in my body for the same thing. I am curious about your holistic person I did read up on what they do but none are available in my region. My plan was to eat healthy and try to exercise then hope it will regulate itself. I cant believe how long it takes for the body to get back to normal.
Thanks for your comment its awful for what you suffered and by the sounds of things your on your way to recovery after almost a years of hard work. Keep it up!
Hi Jane,
Glad we can correspond on this. I read that taking birth control pills can restore your body into a rhythm, but I haven’t done that because I have had such side effects from Depo that I don’t want to put anything else like that in my body. I guess if I don’t see any better results in the next 3-6 months I may try to take other avenues.
I went to this woman for help holistically. It was reasonably priced and I think she definitely help jump start things for me. https://www.wholisticallyspeaking.com/about.html
I do think healthy lifestyle will contribute a lot to getting back in order and unfortunately time too…
As am I. I’m happy to know its not just me but its very unfortunate. The depressing part is people are judging me for putting on stupid amount of weight. Yes, I have other stresses in my life. Today was one of my bad days where I slept until 11 in the morning with no motivation but I felt tired. Due to the weight I put on the guy I was seeing dumped me (which shows a lot for him, dumb ass). I’m finding many guys are thinking “I dont care enough to exercise” when that’s not the reality. Its too bad, really. I think I’m an awesome individual despite this horrifying depo experience. I can only compile to take this time for me and to get my s*** together and sort myself out before starting any kind of relationship. I am just sick and tired of people judging me. Grrr!
Thank you for hearing out my outburst.
I took ONE depo shot in August 2012 and I didn’t return for the next one just due to feeling ill the whole time. I thought once after the shot “ran out” I would be ok. Well that stared a long road of other problems. I dropped weight rapidly like about 15 pounds I got down to about 103 pounds. I couldn’t eat due to acid reflux and dull stomach pains. I had rapid heart beat, sweating, body odor, shaking, depression so bad I thought I was dying. Two years later I still don’t feel like myself but I can say there is hope and your body will eventually return to some what normal. Doctors will deny its from the depo all they will say is well it’s out your system and that might be true but what about the after effects women suffer from this drug. I swear all test and blood work come back fine nothing serious but yet I still was feeling like crap. I still haven’t gained the weight I lost back and it’s been almost two years but I’m almost back to my normal weight. I eat better and feel better. Time seems to be the only thing that helped me. I will never deal with this type of birth control again.
Awe Jane, I understand completely. It has definitely been a time where I am just being the best person I can be and being positive because what you give is what you get and even by working at being happy makes you happier. I have my challenging moments too, but people who truly love you for who you are will look past a bit of weight gain. You will get control of it. I read that exercising in short bursts is one of the better ways to work out that way you are not straining your body over an extended period of time. I read that you should drink lots of water, avoid alcohol, processed foods and fruits or anything that is high in sugar (processed or natural). I can say for myself I do my best, but I struggle with it also. Especially since it seems like no matter what I eat my weight remains stuck. However, this is the MOST helpful post I have read so far -https://www.medhelp.org/posts/Weight-Loss-Alternatives/Getting-off-Depo-Provera-because-of-weight-gain/show/23806?page=1 The girl who posts under the name SurferGirlLaguna has the most helpful and positive things to say about recovering from this. Check it out for sure. Please keep writing and I will keep you posted on my progress. Kandace
Hi Valarie,
I had one shot back on 4/30/14 and three days later began experiencing excruciating pain in all my muscles from the waist down (both legs and buttocks) along with joint pain in my hips and knees. The joint pain went away after about two months but the muscle pain (fibro like symptoms) is still severe. Did your fibro like symptoms decrease after getting off this poison?
Hi Valarie,
I had one shot back on 4/30/14 and three days later began experiencing excruciating pain in all my muscles from the waist down (both legs and buttocks) along with joint pain in my hips and knees. The joint pain went away after about two months but the muscle pain (fibro like symptoms) is still severe. Did your fibro like symptoms decrease after getting off this poison?
i had been on depo for about 3 years. My last injection was in april 2014 and was due in july and oct but never went back for them. as soon as i started the depo shot i didnt have another period since. recently with coming off of the depo shot i have just had some symptoms nothing major, headaches more often, back pains, nausea in the mornings only, some slight cramping like my period is going to return soon but i have yet to have a period, the past few days i have had some super light spotting only in the mornings not sure if thats the start of her returning or what. its very unfortunate that alot of us ladies were not told of these nasty effects when we started taking it. i now know to ask doctors of all effects before i ever agree to taking any kind of medication ever again! to all of the ladies on this forum, i really hope everything starts to get better for all of you ladies very soon and to any of you ladies ttc any time soon good luck!!!! thank you for letting me share my experience. if anyone has any questions or any advice on how to get aunt flo back sooner please feel free to contact me!
I read that link you sent me and it suggested some people took Metformin. I went in today and asked the pharmacist about it. He suggested that I should seriously contact my doctor because after 6 months I should not be feeling how I do (especially weight gain). I finally got in to see the Doctor and he said that is the worst idea ever and made me go for a shit ton of blood work. He said after the results comes in he will discuss the options then. Yikes.
Hi Jane,
Ya, I would agree that it isn’t necessary to take Metformin unless you are having major blood sugar problems. I did like how in the articles she talked about zero carbs and the fact that you can get through it. It’s just nice to hear there will eventually be a time when things even out. Let me know how the blood results go.
Kandace
I have been on the depo for a year and before that i was off and on the depo and pills. After I had my first child in 2010 I had an IUD and because of it i got Chronic PID so now I have to watch what I do. I just came off the depo at the end of september. I know that is a very short time but in these weeks I have had about 20-30 lbs AND my breast are constantly sore. I am on the pill so I thought that would help my hormones go back to normal but it hasn’t any suggestions?
Hi, I started on the depo injection when I was 23 after experiencing really heavy periods. I have epilepsy, so the medication I was on at the time clashed really badly with the pill, so the nurse suggested the injection as an alternative. I took it, and for the first couple of years it was fine, effective, no periods so it was fine. Then I noticed I’d put weight on – had to go up a clothes size as my stomach was so bloated – and my breasts were sore. I told this to the nurse the next time I went for the injection and she ummed and ahhed, then asked the date of my last period. I couldn’t tell her as I hadn’t had one *because* of the injection for three years.
She told me it was probably around the time of my pms/period that my boobs were sore and I was bloated. I was reassured and had the injection again. This time I started getting acne, which was put down to the weight gain and my skin getting oily as a result. It seemed like every time I had the injection something else happened.
After being on the depo for five years and all those symptoms, I saw a new nurse who suggested missing a couple of injections – I was single at the time, so didn’t need birth control – to try and regulate my periods, and also for bone density. About a week after I didn’t have it, my periods came back, and boy they came back. I don’t want to overshare but I thought my womb had burst. I was having terrible cramps, felt like I hated myself, gained even more weight, had headaches and had diarrhoea frequently. After about six weeks I went back to the nurse and told her, and she suggested going back on depo because my periods were back.
(Wait, it gets better) I talked about it with her for about an hour, and finally, stupidly went back on the injection. Periods stopped again, no babies, all seemed ok. However a few months ago I saw my doctor and not a nurse (as I have epilepsy they get me in once a year for a chat) and she mentioned the contraception. She looked a bit concerned as I am not on the same anti-seizure meds now as I was when I started using depo. She asked the date of my last period – I’m now 29 – and when I replied that I had no idea because I’ve been on the depo so long, I couldn’t remember except for the six week break.
I swear to God she almost screamed. I haven’t had a normal period in six years, and I think one of the nurses actually got fired about a month after the doctor found out. (I live in a small community, word gets round fast.)
I am now off the depo permanently. My breasts are sore to touch and they ache all the time, I have cramps severely and often, I have frequent diarrhoea and my periods still haven’t come back as compared to last time. I haven’t even had any spotting, which is something especially that worries me.
Btw the acne has calmed down a lot but now I have insomnia seemingly every night and sometimes just don’t get dressed because I feel like there’s no point getting up.
I’ve been under a lot of stress under the last year as well, my dad died suddenly, he had no will so I had to battle that with solicitors for five months, and also had to have a full thickness skin graft in March after burning the skin off the back of my thigh as I was using straighteners and had a seizure.
I know it’s a bit of a “where to start” case, but I just wondered if anyone out there has had any similar issues or even just been in a similar situation. The doctor has said to try and wait out for six months and see if there are any reactions that will affect my epilepsy. I know she’s trying to do the best for my epilepsy in the long run, but I feel really lonely and don’t really know who to talk to. My boyfriend is sympathetic but doesn’t really… get it, having not had periods/contraceptive issues, what with being a man. Obviously. I don’t want to worry my mum as she is having trouble at work and my best friend is currently in France.
I just, like I say, wanted someone to rant at who might understand a bit. I’m sorry if there’s a load of spelling mistakes, I’m writing this on my kindle at 4am so I can’t really type properly. Thanks for reading and if you have any advice I’d be really happy.
Thanks 🙂
Karen, I am 44 and have been on depo for about 20 years. I have just started getting my period a few months ago, but it is light and only 3 days long. It’s just because our hormones are getting goofy and the shot does not have the same impact on flow as it used to. Judging by the side effects of getting off of depo, I think I will opt to stay on it until menopause is over and then maybe there will be more information available as how to minimize the effects. As long as my dexa scan is ok for my age, I don’t see any reason to stop. Your flow may increase dramatically if you stop, so keep that in mind.
Hi,I’m 41 and have taken depo for 9 years, until dvt occurred, I have had inflamed intestines and felt like all organs under ribcage were on fire, constant nausea, sweating,confusion,pain in non dvt leg and groin,arms and shoulders. As I can no longer take any form of birth control due to dvt, I would not be able to regulate my periods with methods provided. I have taken to eating a healthy diet and taking multi vitamins and vit b,healthy seeds and homemade ginger/peppermint tea. I’m glad I found this site as I thought I was going mad thinking it was the effects of warfarin, now I know it isn’t, I cried most of yesterday but feel better today, my daughter has not had her next injection thank goodness, this is not the best form of bc but I thought it was due to having no periods, I look back and I had become a hardfaced, heartless person with no feelings.things are looking up I’m hoping.
sorry Courtney, but the pill is still fake hormones, so it wont straighten your cycles out, only impose a fake cycle that is more predicable than your current post-depo irregularities. To get your very own cycles back to working order will take a lot of healthy living and being off all synthetic drugs. Get all the help you can and keep at it; healthiness is a life long endeavor.
Hi, I’ve been on the depo since February this year 2014 and I’ve taken the injections twice and I’ve stopped .I’ve not seen my menses till date, I’ve also seen some expansion in my breast, stomach, hips. I’m Always tired and my breathing is not consistent, severe abdominal pains and sometimes my stomach. Please i want to have my flowers ( menses ) back to normal so Please How do i get it back
Good morning, My last depo shot was in July 2014. I was due a couple of weeks ago to get another shot, but was negligent in going. In the meantime, my boyfriend and I have decided to have a baby. I know that it depends on the person, etc. but is there ANYTHING that I can do to insure that I will get pregnant sooner than later? Any suggestions would be great. thank you! 🙂
Hi all My name Emma i wrote a post back in Jan i think it was i had my last shot in September 2013 and didn’t get my periods back for along time even had to get the doctor to put me on some tablets to start me of i had my first period in June 2014 omg it was so bad i had to take time of work my period start coming regular every month but sometime they start coming over 2wks and at one point ended up in the ER as the bleeding go that bad i cudnt even move around i still not even sure if im ovulating as with my period starting at different times have not been able to test myself which now there starting to be came more regular im gonna start testing myself i just hope after being on the depo for 8-9 year it hasn’t screwed my body up to bad as im now on my second married and wud like to have a baby with my new husband im just so scared that it has made me infertile i wud advice anyone who is taking the depo to stop taking it and anyone who is thinking about it try something else wish u guys all the luck in the world hope my posts helps 🙂
hello
im so sorry to hear your all having a bad time on the depo shot
well this is my first shot which i had in august and due to run out in 2 weeks
im worried whats to come so far abit of weight gained
im breaking out in spots
i feel pregnant all the time which im not has i have tested
im angry at my partner all the time mood swings and depression
i really hope when the depo wears off that i dont get all the bad side effects
i just want it out of my system
i havent had a period while been on depo
i was on the mirena coil for 4 years and didnt bleed on that so all together i havent bled in 4 years 2 months
will i ever see my cycle because of been on mirena then going straight onto depo i just want to feel normal well im counting down the days till my period comes but iv got a feeling its going to be a while i cant believe how much i miss my period haha
does it matter that i only had one shot? because i only had one shot will i see my body go back to normal faster im not ttc after it wears off i just want my body back to normal after been on bc for a very long time since my child was born
🙂
Hi there,
I’ve just found a source of information (most of it sensible and science-based) about using Depo-Provera. In the Society for Obstetrics and Gynecology of Canada website, Depo is called “Injection” and there is a fairly extensive “Frequently Asked Questions” section.
I’d strongly suggest that all women who are considering starting Depo-Provera read through these first: https://www.sexualityandu.ca/faqs/birth-control#injection
What I have learned could be better explained from reading the concerns and problems that many of you have brought to this important discussion/board are the following:
1) The Depo-Provera shot is a high enough dose that it suppresses your own hormones–that means it prevents ovulation as well as lowering both estrogen and progesterone levels.
2) Some younger women and those who are in perimenopause may not have full suppression of their reproductive hormones–hence they may get heavy flow.
3) Recovery of menstrual cycles following stopping Depo-Provera depends on whether your own reproductive hormones were coordinated and you were ovulatory before starting Depo. Periods are more likely to come back sooner if you are overweight or obese rather than skinny or of normal weight.
4) Those choosing Depo-Provera in perimenopause should probably plan on having the shot every 2 months instead over every 3–because in perimenopause estrogen levels become higher and are less likely to be suppressed by “outside” or treatment-related higher hormone levels.
As someone who had a horrid time on The Pill, I would probably have used Depo-Provera for contraception if I hadn’t found that using a diaphragm conscientiously and with a full dose of vaginal spermicide each intercourse was very effective. (Never a miss in 13 years’ use for heterosexual intercourse).
Hope this helpful,
Jerilynn
Anyone in peri-menopause should be very cautious using depo. PLEASE read sll info on bone density before using depo. Read previous posts on this site and research current and past lawsuits against Pfizer in regard to the bone density issue.
I’ve been on depo for 9 years and found it to be fantastic with no bleeding or side effects. I have however started (past 2 month) to get migraines,weight gain,mood swings, bloating,stomach cramps and have now had a period?! Not sure whats going on- can depo stop working-I’m only 29 so I’m sure it’s not related to my age and menopause-any ideas?
I’m 32, no children, and I first had the depo shot in June, and I continued to have a period. In late August, I started to bleed nonstop. I thought maybe my body just needed to get used to the shot, so foolishly I had another shot in September (still bleeding nonstop since August). Since the second shot, I’ve felt horrible. My legs from my knees down ache, I have bad headaches, I have trouble sleeping, my hair seems to be falling out more, I’ve gained 15 pounds (I’m currently 5’8″ and 150), I feel depressed, I am always tired, emotional, moody, and now my periods are very, very heavy. I will bleed through a super plus tampon and a pad in under three hours. My symptoms seem similar to Hashimoto’s disease or under active thyroid issues. Has anyone experienced what I am? I’m not sure if I need to see an endocrinologist or GYN. I’m in law school, and I have no insurance and no income besides loans, so I’m not sure what is my best/cheapest option. I don’t want a bunch of unnecessary tests, and I don’t trust doctors to make an accurate or cost-effective decision regarding my treatment.
here’s another example of someone reacting badly to the shot. Some tolerate depo OK and others are like the canaries in the coal mine, warning us all about the fundamental unhealthiness of the whole mechanism of action which essentially shuts down the proper functioning of the endocrine system. My advice is to get on a healthy diet and lifestyle including food, sleep, rest, stress management, and No More Fake Hormones. If problems dont sort themselves out and you cant afford to see a naturopathic physician, then pick the brains of your local health food store staff. Look for the more mature people with knowledge. Often they can tell you what a ND would probably recommend. Steer toward PMS formulas rather than generic female tonics and stick with people who have some training on herbs or many years in the health industry. They shd be able to tell you who the good practitioners are in your town as well.
Im 22 years old and for the past 3 or 4 months after I got off the depo I’ve been none stop spotting its every 4 – 7 days that this happens. My last shot of the depo was in May. It’s driving me crazy. I don’t have any other symptoms besides the spotting. I know I’m not pregnant.
Jenny,
Take one day at a time. I have empathy for your loss. My story is somewhere here but I was on Depo for 6 months. During this time I quit my job, My grandmother died of cancer, I had a cancer scare myself and now things are getting to be normal again. I went to the doctor asking what to do. He made me go and get a pregnancy/blood tests done. I gotta go see him in a few days and see what he has to say. But seriously, take one day at a time. I found working with horses helped a lot. I started riding. I still have days where I am so angry/agitated that I cannot stand myself! I’m not sure what else to say but to keep posting on here. It helps. 🙂 Best of Luck!
Hey Kandace,
I’m not sure if you still read these posts. I got news back on blood work and everything is normal. The doc said the depo is called “the hammer” because it literally stops everything. He said he has never seen anyone gain the amount of weight that I did (40 lbs in 5 months). He said the shot is widely used by doctors to prevent people who have history of becoming pregnant. He said in my case I ought to do more of (I forget the technical word) but mechanical contraceptive. He said as far as the weight goes you just gotta burn it off. It took me 4 years to get to 160 pounds so he said expect another 4 years to get back to that weight. He said that being fat isnt the thing anymore but to have clear arteries. He used the example of Philo man where their Genetics are great but they eat shit therefore die at the age of 55. Then you see old 90 year old woman whos been working on the farm all her life. Yes, shes “fat” but shes a healthy kind of fat. He also noted that it will have up to 24 months to have become regular again and I need to go for a Pelvic examination to make sure cysts are not on the ovaries and everything is where it should be. I have nothing else to offer. I hope you have found your way. Eat healthy, drink water, exercise and treat yourself twice a week. I go Wednesday and Sundays :P.
Hi, I’m 43 and I was on the depo -shot up until June 22,2014. I have been on it for 14 yrs and then they took me off of it my problem has become very serious of carrying a lot of fluid. I went to my primary doctor office on oct. 23 2014 because I was having trouble breathing. Well i.m taking more fluid pills then I was when I was on the Depo shot so with in 4 days because I do weight watchers too. I had lost 13.2 lbs of fluid so I need to talk to someone about this topic.
yes we’re still following this thread. Luvinnia’s doctors said that they called depo “the hammer”? how interesting. Too bad he didnt offer more solutions for helping get the weight off than just burn it. Could he be looking at your thyroid function and other hormones for example? Educating you about blood sugar, liver function, and stuff like that? Medical people seem to assume that nobody wants to do much to help themselves and would rather let time do the healing. Well I say why dont we help things along with nutrition, sleep, stress reduction, supplements, and safer more natural types of medicine and birth control. I find many patients (like some who have commented here) who are highly motivated to make extra efforts to recover from depo rather than waiting for time to heal (wanting kids, getting married, work or social life suffering etc).
Lisa Leger, Justisse Method
Lisa,
the hammer is in the medical journals if you go on Google scholar because it shuts everything down. My doc took blood work that tested thyroid function (10% of woman have lower thyroid, therefore, its normal to be slightly below normal) and other hormones The blood work showed my blood sugar, liver function normal. I am 100% normal for blood. I have to go get a Pelvic Examination to make sure the DEPO never caused cysts on the ovaries and then my doc offered diet/nutrition counselling. Note my doc said DEPO was originally issued for woman who are at high risk for pregnancy. He said to stop using chemical birth control and go mechanical. This way when you want kids just take it out 🙂 That is my conclusion. I hope this helps people. I know how angry I am at myself. You live and learn.
Hi, I have been on depo for 3 years and I stopped using it, its been 8 months not using depo and having menstruation every after 2 weeks is this normal because i want to get pregnant
Hi, I posted on here months ago and I thought I’d give an update. I was on depo for three years after I started experiencing nausea on the pill. My doctor told me I was making up the nausea but that I could go on depo and that it is the same thing as the pill. She is a highly respected general practitioner in my area, and I say that because all of what she told me was completely wrong and I want people to know that doctors aren’t gods. First off nausea is a common sign that your birth control has too much estrogen in it for you, and secondly Depo is the exact opposite of the pill – pregesterone instead of estrogen.
Last August 2013 I had my last Depo shot. Starting end of November I became exhausted to the point of being unable to function, and between November and January I gained 30 lbs. I’m 5’5″ and went from 135lbs to 165lbs – I eat healthy and have an active lifestyle, but I don’t diet and I’ve always weighed between 130 and 140 without making an effort more than staying healthy. I experiences constant constipation, dermatographia, my hair thinned so much my hairdresser asked what was going on, became super sensitive to temperature, severe memory fog to the point my husband and i originally fought because id bring up a sensitive subject multiple times and he thought i was just being a jerk, and had extreme issues with physical anxiety (I say physical anxiety because I’d have panic attacks completely unrelated to what I was doing – I am very aware and know how to control anxiety but this was uncontrollable because it waa a physical reaction unrelated to any sort of emotional worrying).
In January it was so bad my husband begged me to go to the Dr. She told me I was at fault and needed to live a healthy lifestyle (which I had not changed), but that maybe I had depression. I asked about Depo and she said there was no way it would be an issue as I was no longer taking it. By May of this year I had been to 5 diffeeent doctors including an allergist and a naturopath and had done everything from giving myself shots of B6 to taking a double dose of allegra based on their recommendations. I refused depression medication and had my doctor tel me and my husband I was in denial and making up symptoms. However she also kept telling me diet was the reason for my constipation but when I explained my diet would look confused and change the subject. I spent thousands on tests and Dr. Visits.
In May I put my foot down with a near naturopath Dr. that was pretty malleable and demanded hypothyroid medication. After extensive research into ky symptoms I thought that I must be one of those people with a range different then the norm, and being very body aware I knew I’d be able to tell if I went hyperthyrois so I figured I had little to lose. She gave it at a very low dose that I tried for a week and didn’t help. At this point I had decided to take my health into my own hands because all the doctors I’d seen had shown they weren’t out to help me but to follow their own biases. So I independently doubled my dose (15 to 30 I believe). I immediately felt better, stopped being constipated,had a normal mood and started losing weight (fyi for those of you looking to lose weight it was at a slow and normal rate about 1.5lbs a week and I still had my healthy lifestyle so it’s not like thyroid meds were a miracle weight loss drug, they just allowed my body to start recovering naturally).
So thyroid seemed like the answer. However one symptom did not go away. I had started bleeding in March and had bled EVERY SINGLE DAY from then until at that time the end of May, and every day the bleeding got heavier and I started having cramps that became more and more severe. The only thing the doctors could say was wait it out, but it had gone on so long and I trustes them so little that I was terrified that I was doing permanent damage and would be unable to have children. So I warily scheduled an appointment with yet another Dr., this time an OBGYN.
Beginning of June I saw him, more than 7 months after this hell started. He lsitened to my story, stared at me for awhile, then asked if I had ever been on dDepo. I said yes and he told me he never prescribes it, it’s extremely toxic, and I was having severe but common symptoms from withdrawal from depo. He said it messes with ALL your hormones and that’s probably why thyroid meds helped me – it messedbup my thyroid function, but he believed once it was out of my system my thyroid would go back to normal.
He did an ultrasound and discovered that the lining to my uterus was so thin the instrument actually couldn’t read it, which was why I was bleeding so heavily and cramping so badly – at this point I was bleeding from the muscle wall. Progeaterone, which is what depo is, strips your uterine wall for your period.
I was very hesitant but he answerd all my questions so thoroughly and took so much time and was so empathetic that I fibally trusted him. He said I could wait it out or take the pill briefly to stabilize my cycle and build back my uterine wall (estrogen builds the wall, opposite of progesterone). Despite bein given terrified of taking for any more hormones I finally decided to try it – I just couldn’t take bleeding any longer it had already been 3 months.
I took the lowest dose possible for two weeks (my bleeding stopped after a week!!!!!) then started having severe anxiety attacks. My OB said that means its too much estrogen for my body so I had to stop. He suggested we see if that had been long enough to jump start my cycle before trying anything else. Turns out it was. I had a normal cycle in June, July and August. My OB told my husband and I that was enough cycles to believe the depo was out of my system and to try for kids.
I immediately got pregnant and I’m now 14 weeks along. I and the baby are super healthy. I had to go off thyroid meds when I became pregnant because I immediately had symptoms of hyperthyroid and my numbers came back super low (ppregnancy hormones can change thyroid function). I’ve actually lost some weight since becoming pregnant which my OB assures me is normal so far, and I think is the result of getting back my normal metabolism while eating slightly less due to nausea. I think my body is healing itself. Interestingly, pregnancy is WAY easier than being sick off depo was, so I feel great. Just wanted to let you know that even with severe symptoms there is a light at the end of the tunnel and to keep fighting until you find a doctor that is intuitive, intelligent, takes you seriously, and that you can trust you. My experience is they are out there but they are rare. Also please share your experiences with depo with everyone you know – it’s kind of a taboo subject and that’s why people are still getting it today – they have no idea. They market depo in a tricky way and the best way to fight back is to swallow your squirmishness and tell everyone what you went through. I put my story on Facebook despite having people like my highly religious mother in law as a “friend.” Good luck everyone! We’ll see what happens hormonally witg me after giving birth, but I have to say so far I have a feeling I’ll be back to my normal healthy self.
Hi E,
I have had all the same problems but my weight is constantly going up and down but I was just wondering how long it took for your periods to come back and how long till you started ovulating again. I only had one shot on june and my partner and I want to have a baby but I am yet to get my periods. Could you shed some light on my situation please.
Thanks Debbie
I started depo 5 years ago- no information was given to me other than it being an effective birth control method. Over the past two years I have seen countless doctors for pain- all over pain. In the past 9 months; I have fractured both my foot and my leg on two separate occasions. After doing some research I really think I need a bone scan but my doctor will not issue one.
I decided to go off of the shot, in hopes of my pain going away, but I am terrified of the side effects- weight gain, mood swings, etc. I’ve tried to make an appointment with my doctor to go over the side effects and my options for birth control going forward but they are booked out until February and my next shot was scheduled for November- so I’m going into this blind.
My question is: has anyone else had such a terrible time getting information from their doctor? And has anyone else experienced bone pain-does it go away after?
I am 50 years old, I started depo when I was 42 as recommended by my doctor due to high blood pressure. It was brilliant, it stopped my period completely, I stopped the injections ever 3 years, my periods came back after abot 12 months and all was fine. The last time I stopped the injections was when I was about 48, my period was horrendous, 7 full days of full-on blood loss, couldn’t sleep, it was so bad it was waking me up. I barely held a 2.5 week break and it would start all over again after 3-4 months of this went down and straight back on the depo. In the last 10 years I have had extreme weight gain and my doc wants to take me off due to probably my periods would be near finished anyway. Can you please tell me what I could expect and how to handle this. Thanks
oh dear – a 50 year old who’s doctor did her no favors giving her depo all these years. Essentially your peri-menopausal years have been complicated even more than they otherwise would have been; now you are both recovering from depo and approaching the cessation of your fertility cycles at the same time. Heavy girls often have imbalances with blood sugar, other hormones, their liver is often struggling. I recommend a serious health kick with plenty of good food, exercise, proper sleep, stress reduction, and so forth. Consider seeing a Naturopathic Doctor to get your hormonal health on track and learn to chart what cycles you have to monitor your results. Stay focused and motivated – best of luck with recovering your health.
Where do you live Colleen? Its a well known fact in the medical community that depo increases risk of osteoporosis. Most Doctors are well aware that the risk factors for osteoporosis include: Fracture (you’ve had 2), and use of Depo (which you have used). visit http://www.osteoporosis.ca or the official osteoporosis site for your country. Go to your Doctor armed with the guidelines and insist on a bone density test.
Lisa in Canada
great story Danielle – gives the others inspiration and also sobers them to the lengths you had to go to get results.
thanks for contributing and I wish you delight in your new little one. Lisa
Thanks for your quick reply, as the doctors here are not quite up to speed on depo and the consequences of its use and I have to say for the years I was on (apart from the weight gain and I do believe it was the depo and not me and it probably won’t come off till I’m off the depo) it served it’s purpose. Should I go off this cold turkey, I do eat healthy and exercise everyday … I’m totally confused and concerned now, it appears this has led to more questions than answers.
read thru the comments, especially those from Dr. Prior and visit her website http://www.cemcor.org as well. She gives lits of really specific suggestions and talks about peri-menopause as well on her website. its all about the endocrinology… and she’s an Endocrinologist. Lisa
I am so glad I am not the only one experiencing all this. I had been on Depo off and on (mostly on) for the last 16-17 years. I had taken a few breaks and never had any problems, but after going off it in September after being on for the last 5 years it has been absolute hell. It started with slight occasional dizziness, feeling muddle-headed, and being lethargic. Then severe depression. The depression lifted quite a bit, but my mental clarity has declined severely. I get confused, I have trouble thinking and focusing on topics, and often am left grasping for words. All this while I am supposed to be applying for a doctoral program!
The dizziness escalated sharply the other day, while I was driving on the highway. I had felt fine the last couple of days and was driving down the road when suddenly I got intensely dizzy – I mean the world suddenly looked like a spinning slot machine wheel. I could focus on nothing further than arm’s reach. I managed to pull over, and it subsided a bit, but I have had dizziness ever since. I cannot drive, I have difficulty walking a lot of the time. I am trapped in a fuzz-filled brain and am always worried I will have another “episode” in public.
I just want to be able to function normally again. I have so much to do – my research, applying for programs, taking the GRE – that I simply cannot do in my current state. The other day I had difficulty figuring out how to operate the shower, of all things! And of course there are the other fun side effects – I have always been around 140 lbs, yet during this last round of Depo I gained 45 lbs. Some of that may have been caused by a broken foot that took forever to heal, during which time I was pretty sedentary. Did they alter the formula or dosage at some point? Every other time I went off Depo I had no problems whatsoever, yet this time I am reduced to being a shut-in who can’t go get groceries by herself.
I received the Depo shot for the first and only time in July 2014. I am 24 years old and this has been the worse experience of my life. The first month went well…My period was shortened, and I felt great. By July I started at 146 lbs and now by November I am up to 158 lbs. I have suffered starting August 12 till October 27 with a continual period that seemed like a never ending flood some days and to a “false hope” spotting of an end on others. I went through massive migraines starting the end of July and still now occasionally suffer from them to the point the doctor put me on several different medications to easy the discomfort which occasionally aided the frequency but not the severity. I begun developing, what the doctor called, cranial edema or cyst on the top of my skull. I was informed by the doctors after blood work, xrays, ct scan, and numerous visits that there is nothing wrong with me, “that the hormone shot just needs to wear off.” It’s been a month since I was supposed to get another one and like the ladies on here have stated this part stinks, but I don’t feel worse then when I was actually one it. Sore breasts, bloating, weight gain (even with proper dieting/exercise), abnormal temperature changes, and slight unexplained depression mood swings. I thought I would share my story and say thank all of you for sharing yours and making me feel not so alone.
I received the Depo shot for the first and only time in July 2014. I am 24 years old and this has been the worse experience of my life. The first month went well…My period was shortened, and I felt great. By July I started at 146 lbs and now by November I am up to 158 lbs. I have suffered starting August 12 till October 27 with a continual period that seemed like a never ending flood some days and to a “false hope” spotting of an end on others. I went through massive migraines starting the end of July and still now occasionally suffer from them to the point the doctor put me on several different medications to easy the discomfort which occasionally aided the frequency but not the severity. I begun developing, what the doctor called, cranial edema or cyst on the top of my skull. I was informed by the doctors after blood work, xrays, ct scan, and numerous visits that there is nothing wrong with me, “that the hormone shot just needs to wear off.” It’s been a month since I was supposed to get another one and like the ladies on here have stated this part stinks, but I don’t feel worse then when I was actually one it. Sore breasts, bloating, menstrual cramps, weight gain (even with proper dieting/exercise), abnormal temperature changes, and slight unexplained depression mood swings. I thought I would share my story and say thank all of you for sharing yours and making me feel not so alone.
I started the depo shot in about October of 2012 when I was 18 years old and I just came off the shot last month (October 2014). Since then I’ve experienced emotional highs and lows. I can go from being extremely angry to laughing or crying a few minutes later. I also have experienced extreme weight gain, I was a size 9 and now I am a size 12. While I know this was over the course of the last few months it makes me extremely irritable. I have yet to have a period and while on the shot I rarely had a period and when I did it was very heavy and irregular. Is there any advice you would give me as a newly married woman, struggling with the stress of being off the shot and with a new promotion?
hi i have been on depo for 17 years i was told to come off it as my bones were affected and full on osteoporosis which i am not happy im only 42 i was hoping i would become pregant but after reading all the info i doubt this i get bloatingness weight gain breasts are always sore and each mth they get worse
I’m scared I’m having bad withdrawals will this get better??? Panic attacks, dizziness, confusion hot flashes, creamy white discharge, dehydration, rapid heart beat. I’m so afraid to drive because I felt dizzy while driving home from work on afternoon.Been on shot for the second time for five years, My last shot was July 28 2014 and due to a lot of things going on in my life I missed my dose for Oct.Not realizing I missed dose. I had blood test and urine test done they found nothing . thanking god because I thought I was having thyroid problems but after reading other comments I’m beginning to think I’m going through withdrawal. Is there any help for this? I’m not going back on depot I believe after finding this page this is what’s wrong with me.
i am glad that i got all the answers to my questions through you,infact i thought i was abnormal but now i understand everything clearly well.you are great.thanks
When I went to my GP to get my first depo shot I had done some research prior to that which prompted me to ask some questions but the doctor at the time dismissed all my queries as nothing to work about without anything to back him up. I reckon there is far too little information available about this shot, and it is given too freely without the side effects being clearly understood. Luckily I kind of knew what I was getting in to since doing some heavy research since my doctor didn’t mention hardly anything and just gave it to me 5 minutes later after me asking for information about it. Unfortunately I wasn’t one of the lucky ones who’s period stopped all together, so near the end of my first 3 months I decided not to continue with it since it wasn’t worth the almost constant (but not heavy) bleeding to me. Luckily I haven’t had any massive side effects other than still bleeding after sex, but its only been less than 2 weeks since i’ve come off it. I’m just glad I didn’t persist with it and end up with horrible side effects like a lot of the commenters have had. I hope all of you have found/will find relief soon! They should definitely make all the possibilities and side effects well known.
I have been on depo for 7yrs straight and i have finally decided to get off cause my doctor told me all my problems came from this depo provera shot…i have gain like 90 pounds in these yrs and suffering from migraine,moodswings,depression,and a lot more other things..Since i been off my cycle have been on for 30 days non stop..I’m so miserable been to the ER so many times and they do nothing but put me some pills called Provera which i think made my period flow alot heavier…I’m so angry about this depo i need help on how to get my cycle back to normal and this weight off…I’m 27yrs old with 3 kids…I really need some help with this please…I’m tired of being happy sad and crying all at the same time i’m losing it please help…
Gosh Brittney – can you see a gyne or Endocrinologist? Sounds like you need personalized care from someone who knows your full medical history and you wont get that at Emerg. In fact the pills called Provera (notice that the shot is Depo-Provera?) might be prolonging your agony.
Do what you can to eat healthy, rest, exercise and reduce stress. You’ve got a project ahead of you to get healthy, but its worth the effort because you’ll feel fantastic compared to now. Consider trying Citrus Bioflavanoids to dry up the prolonged bleeding; it doesnt correct the hormones, but it repairs small capillaries that are leaking blood in the uterine wall. In my clinical experience, it Often works in a couple of days when women take about 2 500mg caps 3 times a day. Once bleeding dries up, probly a good idea to take 2-3 a day for maintenance for a few cycles. This is not a personal prescription, just the type of suggestion I’d make in the pharmacy where I work.
Thanks Lisa i will try that tomorrow cause i’m still on my cycle…I’m so depressed..I got a appt setup with GYN so i will see what she says…I will give you a update soon as i hear anything from them…Thanks for the help!!
What was the name of the pills please Danielle the doctor tried with you? i been on my cycle for over 3o days since i been off the Depo shot…I been off the depo for 7 months now…How long did it take for your cycle to get back to normal?
I took depo one time and decided not to take it again I was bleeding for almost 5months now I spot and have very sharp cramps to where I can’t move my breast are tender my face has broken out secretly I have 25 pounds since my shot and.continue to gain weight I was diagnosed with severe depression as a result of coming off of the shot and my vitamin d levels went down to a 20 so now I take vitamin d pills and we have been trying to conceive and no luck at all I’m sacred I won’t be able to conceive anymore
I took depo one time and decided not to take it again I was bleeding for almost 5months now I spot and have very sharp cramps to where I can’t move my breast are tender my face has broken out secretly I have 25 pounds since my shot and.continue to gain weight I was diagnosed with severe depression as a result of coming off of the shot and my vitamin d levels went down to a 20 so now I take vitamin d pills and we have been trying to conceive and no luck at all I’m sacred I won’t be able to conceive anymore
I have tried the depo several times over the years, alternating with other types of birth control. I received on shot May 27 and was due for the second by August 21. I have not bled on the shot, however, I had a two day period from Sept. 27-29. I have not received a period since then. I have been getting all of those symptoms mentioned above and was convinced I was pregnant. I had taken about four pregnancy tests and all have come back negative. This post helped to ease my mind a lot. Thank you!
Alena
I forgot to mention that I never received the second shot.
I had one dose of depo and it was nothing but problems. I had 4 months of bleeding after the first 2 weeks, female pain, crying spells, mood swing, severe anxiety. I’ve been off the shot for 5 months and I still have these problems aside from the 4 month flow. the mood swings, anxiety and pain have worsened. My periods last 10 days and the flow is abnormal. These symptoms from depo have almost destroyed my relationship several times
I had one dose of depo and it was nothing but problems. I had 4 months of bleeding after the first 2 weeks, female pain, crying spells, mood swing, severe anxiety. I’ve been off the shot for 5 months and I still have these problems aside from the 4 month flow. the mood swings, anxiety and pain have worsened. My periods last 10 days and the flow is abnormal. These symptoms from depo have almost destroyed my relationship several times.I’m also trying to conceive and I’m worried the shot broke me
I’d like to add; I’ve been in the hospital numerous times for the pain
I’d like to add; I’ve been in the hospital numerous times for the pain and I’m concerned I’m unable to conceive.
ihave had the depo for around 19 yrs, loved it and never had problems, ive had no monthlys from day one, my dr said i had been on it to long, so had last one earlier this year, ive had 2 bone scans in 6 years, all ok there as well, i have just recently started getting headaches backache quite badley and nausea i felt so much better on the depo and will be making an app to try to get it again, i am nearly 50 and honestly felt better on it than of
hi valerie, i was on depo for approx 19 yrs, stopped monthlys immediatly, i have never in that time had a problem, i came of it earlier this year may time i think,and this last 2 weeks i have had nausea headaches and awful backache,and im so tired, im nearly 50 now and really considering going back on it, i felt so much better whilst on it, i have had 2 bone scans and they were good, i do wonder if its the menopause which i am going to have blood test done thur next week, bit confused as to what to do really
i was on the depo for almost a year and the last couple of months that i was on it, I’m constantly bleeding anytime i am sexually aroused. i just switched back to the implant about a month ago ( in november 2014) and im still bleeding during and after sex. when i was on the implant this never happened so its obvious this is a effect of the depo. now that ive switched back, when should this awkward bleeding during sex stop?
I was taking depo by month of nov.2013 untill month of june 2014 after my last shot on month of june.i forgot to take a shot againon september,im still waiting for my period to yake another shot but i cannot do because now is month of december untill now i dont have period…i love depo as a contraceptives but have a question??? If still safe to avoid pregnant by dis time or we need to take withdrawal?? Pls some need a help… I want to take a shot again but how?
I had one shot back in September 2014. I had what my doctor classified as “bleeding” but was actually my period for 2 weeks. Then it just stopped and I thought this is awesome. I didn’t suffer mood swings or any of the other side effects. Then about 2-3 weeks before I wasdue for another shot, I started bleeding again. I’ve been bleeding every day for over a month. Some days it’s a litght spotting others I’m needing a pad to contain it instead of a liner. Since my missed shot, I’ve had severe bloating to the point that my clothes that are generally too big for me do not fit. Not to mention the muscle fatigue. Most days I’m lucky if I can lift my arms long enough to get dressed in the morning. I have also been having issues with insomnia, every night I wake up every 2 hours because I can’t stay asleep.
I am 27. I got the Depo shot after having my second healthy child, at age 23. At first I wanted nothing to do with any kind of birth control shot. At all. I actually declined a few times. But after several days of being harassed by my doctor about it and basically talked into getting it, I said ok fine, and I got the shot. I only ended up getting 2 shots. I bled almost continuously for TWO YEARS STRAIGHT(with a couple days break once in a while). I’ve always been thin but for the 1st time ever I was 15 pounds over weight, and my toe
s would turn purple and be very painful, I couldn’t stand long ()
I am 27. I got the Depo shot a few days after having my second child. All normal healthy pregnancy&birth. At first I didn’t want the shot, I told my doctor I didn’t want it, even my husband told her. After being harassed about it for a few days, I finally said ,ok, fine give me the shot. I only went back for 1 more after that, so 2 shots. :'( I bled almost continuously for TWO LONG YEARS STRAIGHT(with a couple days break every couple months when I got lucky. It ruined my sex life. I was an emotional wreck. I was so weak all the time, I couldn’t stand long.. my toes would turn purple and get Very swollen and painful and stay like that months at a time. Not to mention bad headaches and dizziness, sometimes fainting. I got a different doctor, they said I needed exploratory surgery to see what was wrong. I couldn’t afford the surgery and assumed I was stuck that way, but prayed to get healthy again like I was before Depo. Another year and a half went by with my periods gradually becoming almost normal. My toes are usually fine but my knees still have problems and sometimes My legs go numb and sometimes My arms too. I have been trying to get pregnant for a year now but nothing so far. I used to be strong and healthy, but now I am just weak ,tired, can’t sleep for nights in a row sometimes.. :'( Depo shot definitely ruined my health and maybe even my chance to ever have a son. In and also the headaches and dizziness never went away and my breasts are half the size they were, and I have thinning hair. Depo may have caused me cancer. I think Every woman,of all ages and situations, should stay away from the Depo destruction shot and I hope I am the worst case scenario in this
Hi,
I recently made the descison to stop my depo injection. I have been on the depo injection for 8 years. I was due my shot on 3rd December 2014. It’s now been 3 or so since that date. The last week I have been experiencing extreme bloated feelings, extreme tummy pains and have been feeling constantly sick for the 2/3 days! Has anyone else had this and is this normal?!
Hi,
I recently made the descison to stop my depo injection. I have been on the depo injection for 8 years. I was due my shot on 3rd December 2014. It’s now been 3 weeks or so since that date. The last week I have been experiencing extreme bloated feelings, extreme tummy pains and have been feeling constantly sick for the 2/3 days! Has anyone else had this and is this normal?!
So the part on why some women experience more or less bleeding is believed to be caused by amount of stress and how much weight the person has gained and rather they are older or younger I think is completely wrong. I’m 20 years old havent gained any weight since I’ve been on the shot (almost 9 months) and I have had quite a bit of stress. I’ve been on my period for over a month now. Very heavy which is not a normal thing for me.
Hi ladies I have been on the depo on and off for 13 years first time I was on it was after I had my son and I was on it for about 8 years had no problems then met my future husband and year later we decided we wanted a baby so I went off the shot took about 9 months before I got my first period then 2 months later I got pregnant with my beautiful daughter. Then when I had my son 3 moths after I had him I went back on the depo yet again no problems then a few reddish brownish discharges very unusual for me. Missed December 2013 didn’t get it till January decided couldn’t be bothered with it any more and haven’t had it since then. Last few months had bleeding one day not allot just a few spots so thinking maybe period but not sure. Last month 28 days later than the other weird thing I had bleeding one day then nothing then the next day light bleeding for 4 days later. Had unprotected sex on Xmas day due on I think on the 30th. Yesterday light bleeding went threw knickers sorry tmi. But not enough for a pad and stopped later that day nothing so far today. Is this a period or what could this be …. Thanks for reading.
Hi ladies I have been on the depo on and off for 13 years first time I was on it was after I had my son and I was on it for about 8 years had no problems then met my future husband and year later we decided we wanted a baby so I went off the shot took aboutt 9 months before I got my first period then 2 months later I got pregnant with my beautiful daughter. Then when I had my son 3 moths after I had him I went back on the depo yet again no problems then a few reddish brownish discharges very unusual for me. Missed December 2013 didn’t get it till January decided couldn’t be bothered with it any more and haven’t had it since then. Last few months had bleeding one day not allot just a few spots so thinking maybe period but not sure. Last month 28 days later than the other weird thing I had bleeding one day then nothing then the next day light bleeding for 4 days later. Had unprotected sex on Xmas day due on I think on the 30th. Yesterday light bleeding went threw knickers sorry tmi. But not enough for a pad and stopped later that day nothing so far today. Is this a period or what could this be …. Thanks for reading.
I took depo off and on for 10 years. I am, today actually, 28 and I stopped taking it a year and half ago and have yet to have a period. I have hot flashes, night sweats, EXTREME moodiness and am starting to think I’m PRE,MENOPAUSAL AT 28!!!!
ok so I read your blog but it had nothing in there about how the depo can cause a women to have cythes on there overies. The reasion I am pointing this out is because that is the main reasion I stopped taking the depo 4 months ago and still have not started my period and know I am starting to have sharp pains in my uterius on the right side even though the cyth is on my left side. I was also talking to on of my friends and his wife was also on the depo and experionsed the same thing I am going through and she had to go to the hospital so the doctors can force her period to come through so the pain would stop. If all of this is deals with the depo shot then why don’t the doctors explane the symptoms and side effects before wemone gets it because I know for a fact that I did not here my docter say one word of possibly getting a cyth on the overies or not getting your period aftter taking it and then having sharp pains while wating to see if you do get your period.
I am so sorry to hear all of the horror stories from so many women. I got off the Depo in Oct. and still no period. I gained 20 lbs and have nausea and heartburn nearly every day. I have breast tenderness and discharge as well. Just very uncomfortable and not my usual self. i hope to get back to normal soon, but I am afraid that is not going to happen. I am afraid to get my period just from reading all of these blogs. I do feel that I am pregnant, but I am sure I am not. Just having the symptoms. It is pretty crappy that we all got this shot to prevent pregnancy and are now all ending up with terrible side effects and some of us that want to get pregnant can’t.
I think it is important to note that not all women have these side effects. After being on depo for over 20 years, I had my last injection January 2014. Nine months later I had a regular period of light to medium flow for three days a month. Fortunately, I have had no problems getting off of the depo. I was afraid of coming off of it because of all the posts.
I have been 6 months post depo and this is the first week my anxiety has suddenly stopped after I felt it for months. I now have random tender breasts along with a fluttering in my stomach even when I have had no sex due to zero sex drive while I was on depo! This is one if the most strangest experiences. Feeling pregnant with all the symptoms, toilet to wee a lot more, fluttering in my stomach, i can smell everything stronger than usual and eating loads! Almost 7 months post depo and NOT actually pregnant at all.
I was on Depo for 2 years and have been off Depo since September 2014, I had 2 months light periods and no side effects. Then just this last two weeks I have had extreme nausea, loss of energy – wanting to sleep all the time, headaches, sore breasts and I also have a funny taste in my mouth all the time and I have gained at least 7kgs in two months. There is no way that I am pregnant. I have not got my period again yet, but are hoping to so my body can be normal again. I wish I had never taken this shot. I feel for all of us suffering from these side effects, and you are not alone.
I’m 18 years old. I had my first and only shot on october 2, 2014 on november 11th I miscarried at 5 and a half weeks! My boyfriend and I used condoms most of the time but didn’t a few times and I ended up pregnant. I had no idea I was pregnant because I thought the nausea I had been feeling was from the shot. My doctor gave me a urine test but at 1-2 weeks you can not get a positive on a urine test! I still grieve and regret ever taking this damn shot. Also I am now on the pill (1st pack, day four of the last row) and still no period. I have gained 20 pounds in the past 4-5 months making me almost 200 pounds ( I’m about 5’9″ tall). In my opinion this shot shouldn’t have ever been created and it should be manditory for a blood pregnancy test especially if you tell your doctor you have a period 4 weeks before and you have had unprotected sex! This shot has almost ruined my relationship many times because of my miscarriage, bipolar like moods and the depression I have expierenced. If you are reading this and thinking about getting the depo, dont! It’s not worth it. Stick with the implant or pill.
I have the exact same symptoms when stopping and i recently stopped the depo. anything helping you or any advise you could give??
I am 30 years old & was on the depo for 7 years. Last shot was August 2013. Had one period 6 months later but teen nothing. I went to OB/GYN after a year & she put me on BC which was miserable. I took myself off that & had 3 periods after that but now nothing. In the meantime the “side effects” have been miserable: sore breasts, night sweats, nauseau, no sleep, smells make me vomit, headaches, mood swings, shakiness… The list goes on. We have been TTC for over a year. We have one child already so I know I used to ovulate. I am frustrated that I was not made aware of how hard it is to get my body back to its normal. I’ve been off the depo for 18 months & TTC for a year now. How long before I should go back to the doctor & what should I ask them to do? I really don’t want on BC because of how it makes me feel.
Hi Sarah,
I’ve copied and pasted the part of this post that is relevant to your situation. You can download the information on Cyclic Progesterone Therapy and take it to your doctor. Here is the link for that:
https://www.cemcor.ubc.ca/resources/cyclic-progesterone-therapy
Good luck with your return to fertility
Excerpt from post:
No flow for three months after stopping Depo: I suggest starting to take natural, bio-identical progesterone (see Cyclic Progesterone Therapy) for two weeks and stop for two weeks. Don’t be discouraged if you don’t get a period when you stop it. Just keep doing that two weeks “on” and two weeks “off” progesterone until your flow returns. Even without flow, this treatment will increase bone density (based on a trial we did years ago).
If, in the course of taking cyclic progesterone you start getting irregular flow, follow the instructions (and picture) in that handout carefully. Most of all, think of this as restoring a normal balance of your own hormones and ovulatory menstrual cycles.
When you start noticing stretchy mucus about the middle of the month, this means your estrogen levels are recovering. Now you can actively start working on becoming pregnant, if this is your desire. You will take the progesterone for two weeks or fourteen days but start checking for your urinary LH peak (with a fertility kit you can buy over the counter) in the evening when you notice stretchy vaginal mucus. Only begin the progesterone after you see the LH peak (a positive test) or after the stretchy mucus decreases. The reason is that if you take the progesterone too early it could suppress that necessary LH peak.
I just went on the Depo shot only a few weeks ago and my main side effect has been: depression. Its awful. I am typically a very happy, positive, and optimistic person. I rarely would have a bad day. And now I count a good day if it was just “OK” and I didn’t cry all day. I am irritable and just severely apathetic and cry a lot. I have ZERO and I mean ZERO sex drive.
I don’t know what to do. I can’t believe I am going to feel like this for 3 or maybe more! months.
Does anyone know of any way to combat these side effects? I also have new terrible acne. But I’d rather have a red face than feel like this.
I just started tsking depo 3 months ago and i have thick hair on my chin, please advice, i want to stop this short this my next appointment is on the 16 march and dont intend on going back, will this corse hair on my chin go away. i was never like this untill i started Depo
Has the bleeding stopped since you went off of the shot? I have nonstop spotting and I am not going to get another injection (which is scheduled for the next week or two) and I am wanting to know when the spotting will stop being constant.
Aside from tinkering with hormones (which is what got you into this mess in the first place), I would suggest taking a B vitamin complex and consider adding fish oil and a calcium/magnesium supplement.
The bleeding has stopped. Been off depo for 10 months and still haven’t had a normal period. In January I had brown spotting 10 days after my period stopped.
Most horrible thing I have ever given my body. My doctor put me on depro right after having my baby @ 33 years old. Went off of it after taking 7 injections. Took 6 months to get a cycle every two weeks and there heavy. Breast very tender, and morning hot flashes daily. Terrifying experience and my doctor is telling me to wait it out. Not too mention the 30 pounds I put on with it. There needs to be something done with this needle. The side affects totally weigh out the cons far more than the pros of taking it.
I had terrible depression with my first injection. I am prone to anxiety and slight depression and the Depo seemed to magnify it. I am on Lexapro now and feel much better. Hang in there and talk to your doctor!
Get blood work done. I have been eating a lot, along with other problems.
I recently got checked and my testosterone level is high to the depo. I’ve been off it since june and things haven’t returned to normal
Hi i was on the depo shot for close to a year and I got off of it and now haven’t had a period for 1year I’m 23 years old I need to know if this is normal or not
I was taking depo for last 7 years and was pretty much ok. From last August decided to off. From end of January having period and its continuing. After every three days it shows complete. Just one night then again starts fresh flow from morning. Should I start pill to regular it?
I’ve had blood work, ultrasounds,and catscans done.Nobody seems to know why I’m having pain,I see a specialist in a couple weeks
I was taking depo for 9 mmonths.december last year decided to stop.when will i have my period again?help plsss.
Started the depo may of 2014. Since then I gained 20 pounds and have too many stretchmarks. I have no desire to do anything but sleep and eat. I’m constantly hungry and tired. Before the shot I was barely over 100lbs and happy go lucky. Nowadays I couldn’t careless about being active or having fun basically. On February 5th I was supposed to go and get my shot but I didn’t due to how miserable I am from it. (Not to mention hip and back pain.) My periods are terrible therefore I’ve been on birthcontrol for years. Nothing has been so terrible Like the shot. I haven’t bled yet surprisingly. But I am looking to get pregnant soon so I am hoping things will get back on track. I wouldn’t recommend the depo shot to anyone! Most depressing thing in my life. Does anyone know the usual amount of time after quitting that pregnancy occurs?
Hi Kerri, I too am having those same symptons. I was on depo for 8 years and advised by my doctor it was time to get off it. Last shot was in August 2014 I have not had my period since but really don’t expect it as I’m nearly 51 and don’t want it. But late December I started to have severe abdominal pain, bloating, constipation and generally feeling yucky. All blood tests came back normal, going for a ultrasound next week. More fibre in my diet has helped it dramaticaly but still just don’t feel right. I believe now it’s due to the depo and I may need to just wait it out. Good Luck!
I stopped taking the depo shots 7 months ago. I was 19 when I was taking it I am now 20. I was only on it for about a year. As soon as i switched back onto the pills my periods are 10 days apart, not joking sometimes less. I feel like I have my period for almost the whole month. I feel extremely emotional, always up and down. I feel like I can cry so easily. My anxiety has been some what okay. I don’t know what to do and would appreciate some suggestions. Should I go to the doctor and get my hormone levels checked? Ive been back on the pill for going on 8 months and my period is not back to normal, I feel like i’m going to go crazy, I just want to cry. Someone please give some suggestions? Should I go to the doctor and get hormone levels checked? What should I do? I feel to young to be going through this.
First thing you need to understand is that those “periods” you’re talking about are not periods. The pill suppresses the normal ovulation cycle and therefore women on the pill Do Not have normal menstruation. The bleed we have on the pill is fake; its a result of the synthetic hormones and the way they impact our very own hormones. When you have excessive bleeding on the pill, its usually a sign of too much synthetic estrogen, but can be other reasons, too. Sounds like you’re not a great candidate for hormonal birth control. Maybe you should consider using barrier methods combined with fertility awareness to avoid pregnancy and let your natural hormones settle down to their normal levels. Check out http://www.justisse.ca for an educational app that helps you learn how to chart your cycles effectively.
Hey. I had one shot of depo last sept. And I only had one it made me really angry and agitated and the littlest things but now I have been bleeding non stop since November is this ever going to end. I already prior was anemic and iron deficient. I honestly wasn’t informed about any of these side affects. I only got the shot for abdominal pain after months of pain from a gallbladder removal. I just want to know being 23 and 5’6 155 pounds will this ever stop I was really regular prior to the shot and now it’s just getting worse. People have said that going on a pill birth control will regulate you again but workin in a medical field I have seen many women who end up with blood clots in their lungs from them. Please help me out here it is getting really old
Hello Breanne so you got the shot to help with pain from having your gallbladder removed? This shot actually gives women gallbladder trouble along with a list of others issues. I’m just wondering who advised you it would be a good idea to get the shot for that? Also birth control harms the gallbladder and that could be why you had to get it removed in the first place. I took only one shot 2 years ago and I still have problems
i had my gallbladder out in April I got the shot in September to help with abdominal discomfort. Which it did for a week or so they said it would lower the inflammation in my abdomen. I just was wanting to know if there was anything like going on a different birth control and get the bleeding regulated and then maybe hopefully get to wein myself off of it completely because I want to start having children and start that part of my life. Any thoughts and advice would be very appreciated
I have been on the depo for 2 years now my next shot is due in a few weeks. for the first year and a half on the shot i bled almost constantly. then all of a sudden i stopped. im constantly tired and always yelling and angry at anything and everything. i have NO sex drive. only in the last few months have i gained about 15 lbs. I have no desire to do anything at all cook, clean, take care of anything. I was debating going off it to see if it helps but after reading some of y’alls withdraw symptoms I dont know if i should or shouldnt. it almost sounds worse to go off then to stay on. i dont konw what do you think?
Breanne says that she had her gall bladder out recently. Does anyone notice that gall bladder disease is a risk of hormonal contraceptives? This seems to be lost in the rush to recommend these drugs. As a fertility educator, I’d advise refraining from hormonal methods. let your natural fertility cycles return to normal and then begin your family when your health returns.
i went to a new gyno and they said they don’t even recommend the shot due to all the awful side effects. They gave me the option of either letting the bleeding stop on its own they say usually 6 months and I am on month 4 and if I wanted to do the Nuva ring that is also an option. It will thicken the uterine walls again since while on the depo it thins them to prevent sperm from impregnating you. I do want to clarify that I had my Gallbladder out BEFORE I was introduced to the depo shot to help with inflammation in my abdomen. But the doc i have seen today says it can lead to chloestatsis (Gallbladder issues) so if I can say anything stop taking this awful conceptive and let your body adjust to something else
Best of luck ladies
This was my first time taking the shot. Currently I’m on the withdrawl side now. I liked being on the shot because I felt protected and didn’t have to take the pill everyday. Now, I’ve been having spotting and randomly bleeding for a week. The worst thing is I don’t know if it’s my period. One day I would have a drip of blood the next day a pool of it. It’s been going on and off. Also, for the past 2 weeks now I’ve been crazy moody. I’ve been getting pissed faster and sad at times more than usual. Definitely not taking this again and going back to my natural flow when it eventually comes back.
It can take up to one year for things to return to normal after depo
I am 41 and took the depo for 13 years. I gained weight, suffered from bouts of mild depression and became disconnected from my feelings. I started to realise things weren’t right and so chose to stop taking it. My last shot was February 2014 – 9 months ago. I initially had the bloating, sore breasts, hot flashes and aching. I then had weight gain which I worked very hard to keep at 7 pounds only, sore and swollen breasts and stomach, periods of depression where I couldn’t get out of bed, severe anxiety and then in September a lot of my hair fell out. This is apparently very common after coming off any birth control. I had blood tests for everything and all came back normal aside from my hormones slightly imbalanced but not enough to treat. I’m not peri menopausal either. Now after 9 months the weight has just started to come off and my relationship to food has changed completely. I want to eat healthily and nowhere near the amount I wanted to eat whilst on, and since coming off, depo. I have anxiety briefly around the start of my cycle but otherwise am fine. My hair has new growth but I understand that can take a year to resolve after the shed. The hair loss is diffuse, without bald patches, and I found that Nizoral and baby shampoo helped. My periods returned last august and I was on a 7 day cycle for 3 months. I’m now on a 20-25 day cycle which is too short but is settling down. In myself I don’t feel depressed any more and I feel more connected to my body, feelings and emotions than I have for years. I really wish I had never touched depo or come off it much sooner. I do think it is important to allow your body to settle down naturally however difficult the journey through that might be. I now feel better than I have for years and things do get better after stopping depo but it does take time. I did a lot of research but ultimately I decided to listen to my body and what it needed. Exercise does help but I couldn’t face it. Instead I took my exercise in the form of long walks outside and gentle yoga. Both helped immensely for my body and my state of mind. For the anxiety I learned to focus on something that makes me happy and recall every detail of it. It focuses the mind and calms the anxiety so that it is manageable when you feel it. Each day I feel better and more like myself and it is absolutely worth pushing through the difficult period in order to come out the other side. It’s difficult to find the experience of people who have come through this and are out the side and feeling better so thought I would contribute. It absolutely does get better and having learned to listen to my body- every ache, soreness and symptom – I now feel very aware of my emotions, state of mind and general well being and I am very thankful for that. I feel stronger, more balanced and more in control than I can remember and I feel extremely positive. Hopefully this post helps you believe that it is worth pushing through and motivates you to get through those difficult days.
Hi, so I was bleeding since the beginning of Feb and the due date is on Feb 26, but I switched to Birth Control Pills on that day and then my spotting had stop. I was wondering did the pills cause it to stop?
I had stopped taking depo-Vera for approximately 7 months I was on my cycle when I decided to get back on and unfortunately this has been my longest cycle thus far I am going on 3 weeks now. Previously when I was on drop I did not have a cycle at all so now I am wondering why is it that my body is not reacting the same to the drug?
Ho, I have a question, I took my depo provera shot (for first time, never been on any birth control before) the first day of my period and the day after my period was gone….it’s that normal? Does that means that depo is working in my body? How long do I have to wait to have an intercourse? I’m irregular so I also want to know if depo will be effective on me after 24 hours….
I have been on Depo Provera for about 6-8 years. I decided this past December to stop taking it as I’m 48 thus getting close to the big 50 and menopause, plus I was starting to have a hard time dealing with the side effects. I’ve had a period for off and on for 2 weeks now. I was experiencing symptoms like I had a bladder infection. Went to the GP for tests and I did not have one. Those feeling have gone away now. I gained about 20 pounds while on Depo and hope they come off, however, I’ve read once you’ve gained the weight it will not come off. I’ve noticed the past week that I have nausea on and off. I can’t stand it. Honestly I wish I never started on this drug and warn those who want to go on it. Exhaust all other possibilities before going on it. As far as I’m concerned this stuff is poison and should no longer be available.
When I was 13, I had one does of the Depo Provera shot and my period has not been normal since. I am now 19 and I can maybe count on two hands how many periods I’ve had in the last 6, almost 7 years. My gynecologist put me on the birth control pill about 3 years ago and told me it will run its course and my period will regulate itself, but that’s not the case. I stopped the pill about 2 years ago. I will bleed on and off from time to time, but it is more like spotting. I like to think my period is going to come and be normal, but it never does. My boyfriend and I have been trying to have a baby, but I don’t even think that is possible anymore based on what the Depo shot has done to my reproductive system. Can you give me advice on what I should do?
When I was 13, I had one dose of the Depo Provera shot and my period has not been normal since. I am now 19 and I can maybe count on two hands how many periods I’ve had in the last 6, almost 7 years. My gynecologist put me on the birth control pill about 3 years ago and told me it will run its course and my period will regulate itself, but that’s not the case. I stopped the pill about 2 years ago. I will bleed on and off from time to time, but it is more like spotting. I like to think my period is going to come and be normal, but it never does. My boyfriend and I have been trying to have a baby, but I don’t even think that is possible anymore based on what the Depo shot has done to my reproductive system. Can you give me advice on what I should do?
Spotting does not mean you arae infertile.
You can have that checked out my a fertility specialists.
You spotting is not from the depo but probably because of your pill and having intercourse.
You will need to stop having intercourse to see any affect.
Also, having a child at 19 may add onto the stress of your body due to your age and could prolong issues.
See a specialist.
I stopped depo after 19 years. I am 34 now. My period returned, I did not gain weight (on or off depo; I am really athletic), my skin looks better, but other problems have developed. I have an ovarian cyst that was found after abdominal pain and pain with intercourse. I have also experienced indigestion and nausea at the start of my period. A pelvic ultrasound showed an additional abnormal area not related to the cyst. I wonder if depo may have kept issues like endometriosis and ovarian cysts in check by limiting the amount of my hormones. Now that research indicates that depo is ok for my bones, I’m thinking about starting back on it after a long discussion with my husband about children.
Any advice would be greatly appreciated. I feel that my PA is stumped and my insurance requires care through the university where I work. Is this worth seeing a specialist?
Just a question being post depo for approx a year now and having nausea, sore breasts and irregular periods how long on average have people found it has taken for the side effects to disappear? I was on the depo for 8-10 years.
Wow, this article and the comments explain a lot… my last shot was at the beginning of August 2014 and would have worn off in November- I was on it for about 2.5 years. Since we are trying to conceive, I keep thinking we’ve gotten pregnant but tests keep coming back as negative. It’s really disheartening. Same kind of symptoms- tender, swollen breasts, mood swings, hot flushes, constipation, increased appetite… sigh. I’m 26 and am hoping this doesn’t last long. Four months into these symptoms and I’m ready to strangle the manufacturer of this drug.
Oh god, I can’t forget the nausea. HOW COULD I FORGET.
I have been on depot for 14yrs and apart from gaining weight had no problems. My injection was due 3 weeks ago but there were no supplies in the chemists!! As I am now 50yrs old and been thinking of coming off it soon I let nature take it course. Now my breasts are so tender I can’t touch them, headaches and a few days of feeling really miserable! I obviously are near the menopause but am so confused as what to do.just wondering if anyone else my age has had these withdrawal symptoms so soon after stopping the injection.x
I got on depo 2 years ago and gained 30 lbs in that time- 17 of them were in my first 3 months of taking depo. I’m getting off it now because the weight gain was so horrible and I am having awful side affects- nausea, vomiting, shakiness, cramps, headache, fatigue…everything you can think of and it hasn’t even been a month yet. I still havent received my period and read that the weight will start to come off once I do. Is there any advice out there? How can I make these withdrawal symptoms go away and how can I speed up the weight loss?
Was on the shot for fifth teen years. Broke my leg last year very easily. Bone density is terrible so I decided to stop last Oct.I had migraine all Dec.I am now in my fourth month of severe nausea. Lost 15 pounds. Can barely function. When will this end?
When will the headaches end? Last shot in January. This is awful. I have also gained 30lbs!!!
I had used depo on and off for almost 7 yrs. Then decided to stop toi become pregnant, witch I did within 1 month. After delivery I was sent home back on depo and was on it for another yr, eventually started to gain weight like crazy, so I stopped Depo for that reason. Within the first 2months I started having really bad hot flashes and dizziness and accelerated heart rate! After 3 months I suffered my 1st horrible panic attack. After that I was getting extremely depressed and anxiety continued.The heart rate issue was so bad I when to a cardiologist but everything checked out fine. When I figured that maybe it was because of stopping the depo, I got back on it due to feel of living this life. Its going to be 1 year soon and even though im still on depo, i still have anxiety symptoms. It is frustrating to not have help.
I have the same exact thing. Worse feeling in the world not being able to control it. I wish there was a way to end this anxiety.
Yes out of all this, I think anxiety and panic attacks are the worst. And I have not once taken any medication for these things because I try to control it my self instead but it is just so hard sometimes…. I wonder when will it end? Literally almost a year I’ve gone thought this suffering. I’m afraid of going far from home because I don’t know when it can happen since it happenes out of nowhere. I’ve had plenty of them that randomly happen during grocery shopping, at work, ect. Before even at home I would get like that, to the point were i would consider calling an ambulance for help.But now at home I feel nervousness but doesn’t really go past that, but its still hard to deal with. But although the anxiety, nervousness, mood changes, are so random, I feel like if ive developed a fear to go out, to travel, to do things in public, things that before I would do just fine or things that before I would enjoy doing, now I try to avoid. And all combined is like living hell. Anyone that is going thru this or has in the past will know what I mean and will understand.
I’ve been on the depo shot for 10 years now(after bwing on the pill from age 16 to 24 for irregular & extremely heavy periods). The 1st three months after my first shot were terrible..I literally bled on and off for 3 months. But after that and over the years, my period has basically disappeared, to where I only spot/have small period on the 2 weeks before my next shot is due. The last 8 months, I’ve only spotted 2 times. Never gained any weight,although my libido did drop drastically over the years. I couldn’t switch to other BC because I’m a smoker, as was worried about the bone density problem(and am not so sure about the IUD). I’m now 34 & we’ve decided we want one more child, so I’m not getting my next shot. My doctor always gives me a 10-day window to get my shot, & in 10 years, I’ve always received my next round the day before or day of for the first available date. That would have been April 4(today is now the 10th), & for the past 3 weeks, I’ve had incredibly sore breasts (taking off my bra at night is the WORST).The last week, I’ve been nauseaus, had terrible gas at night only, & the last 2 days, terrible pain in my abdomen that is a combination of cramps/sharp pain(the ONLY thing that helps is a heating pad applied the majority of the day & night). I thought for sure I was pregnant, but tests came back negative. It makes sense that estrogen levels would be peaking, after 10 years of being suppressed…so glad to have found someone who could break down exactly what’s going on!
I’m 23 years old and was on the shot from 13-17, I missed one of my shots and got pregnant with my son. I went back on the shot as soon as possible after having him. My son was born with down syndrome which doesn’t run in the family and is so strange as I was so young. I don’t think it has anything to do with the shot either. I decided to go off the shot in June 2014 because it’s just really not that good for you and I don’t really have enough calcium in my diet to balance it out. In September I ended up getting a period that lasted an entire month which was awful! I had the worst headaches of my life and my body was in what seemed to be withdrawal from the shot. I’ve read in many online commentaries that it can take up to a year for your body to go back to normal. My cycle is so out of wack, I can have a period every two weeks then not one for an entire month. Depo is the worst thing that has ever happened to me! I’ve always been a really laid back down to earth girl, always hanging out with the guys. But this past month I’ve found my moods changed, I’m starting to have “feelings” and be emotional/moody. I’m wondering if depo messed with my hormones so much and made them so low I never truly felt the way a woman should “feel”. I like the way I’ve always been and I don’t want to have these “feelings” at this point in my life. Can anyone else relate or give me some advice? I’d also like to be on birth control again, one preferably that would stop me from having a cycle because that’s kind of cool. What are your thoughts?
To Sam, I’d like to say that I can relate in the part were u say you feel emotions different, because I used to be nice, but careless in some occasions and pretty tough in some areas that now I think I feel different about( softer feelings) I guess I can say I do see a change in my feelings and moods too.
i am 18 years old. i was on the shot for a year. ive gained 40 pounds and ive had my period every other week since i quit the shot in feb. I was diagnosed with social anxiety and ibs shortly after starting my shot and I’ve been suffering with panic attacks and stomach issuses. Realated?..maybe. I’ve been taking prenatal/calicum pills since I started the shot, to help fight against losing bone density. Even with the pills my bones felt weaker.
i wish i never wouldve done that to my body. im so messed up because of this shot. im calling my doctor monday. yeah, the shot was 100% effective of preventing pregnancy. but honestly its not worth it! I would have rather gotten pregnant.
Hi I’ve been on depo for 8 years now and I’ve had to recently come off of it. A year ago I started levothyroxine and lost a lot of weight. Since then I noticed my weight going up and down and have had a lot of cramping. My dr said my period was trying to come so I got off depo. 6 months after last injection I got my period. It’s irregular and I know it will be. I still have very bad cramps and sometimes they are so severe that I can’t move. I’m just wondering since I’ve had my period already when will the bloating go away? My dr said after a few periods it will but I want to know for sure. Just wondering if you can help me ?